Insurance Blog
Disclaimer
The views, information, and comments in this blog should be understood as the personal opinions of the author and provide only a simplified description of coverages and is not a statement of contract. Insurance products and coverages may not apply in all states.
The Big Beautiful Law of Tax Changes
Thursday, July 17, 2025 1 Stop Benefits & Gork
 Key Updates for Businesses and Individuals - Effective 2025
For Businesses
Key Updates for Businesses and Individuals - Effective 2025
For Businesses
- Corporate Tax Rate reduced to 15%.
- 100% Bonus Depreciation restored for qualifying assets.
- Section 179 Expensing limit increased to $2.5 million.
- Immediate R&D expensing reinstated and made permanent.
- 20% Pass-Through Deduction (Section 199A) made permanent.
- QSBS gain exclusion expanded: 50% (3 years), 75% (4 years), 100% (5+ years).
- Opportunity Zones policy made permanent starting 2027.
- Employer-Provided Childcare Credits increased to 40% (50% for small businesses), max $500,000 ($600,000 for small businesses).
- Charitable Deduction floor set at 1% for C corporations.
- Excess Business Loss Limitation made permanent: $313,000 (single), $626,000 (joint).
- Clean Energy Credits terminated for commercial vehicles post-September 30, 2025.
- Endowment excise tax for private colleges increased to up to 8%.
- PTET deductions preserved for SALT cap workarounds.
- Income Tax Rates (10%-37%) made permanent, with inflation adjustments from 2026.
- Standard Deduction increased: $15,750 (single), $23,625 (head of household), $31,500 (joint) for 2025.
- SALT Deduction cap raised to $40,000 (2025-2029), reverts to $10,000 in 2030.
- Social Security benefits tax eliminated with a $6,000 deduction (2025-2028).
- Tip Income Deduction up to $25,000 (2025-2028).
- Overtime Income Deduction up to $12,500 ($25,000 joint) (2025-2028).
- Car Loan Interest Deduction up to $10,000 (2025-2028).
- Child Tax Credit increased to $2,200, with $1,700 refundable, adjusted for inflation.
- Adoption Tax Credit: $5,000 refundable of $17,280, adjusted for inflation.
- 529 Plan distributions expanded to $20,000 for K-12 expenses.
- Trump Accounts: $1,000 tax-exempt savings for children born 2025-2029.
- Estate Tax exemption increased to $15 million (individuals), adjusted for inflation.
- Personal Exemptions permanently eliminated, except for seniors.
- Clean Energy Credits terminated for EVs and charging equipment post-2025.
- Dependent Care Assistance limit increased to $7,500 after 2025.
- Charitable Deduction floor set at 0.5% for itemizers.
- Moving Expenses deduction permanently repealed, except for Armed Forces.
Understanding the New ICHRA Rules Under the One Big Beautiful Bill Act: A Game-Changer for Employers
Wednesday, July 16, 2025 1 Stop Benefits, Inc. and Grok
 Understanding the New ICHRA Rules Under the One Big Beautiful Bill Act: A Game-Changer for Employers
The One Big Beautiful Bill Act (OBBBA), signed into law on July 4, 2025, has brought significant changes to employee benefits, including updates to Individual Coverage Health Reimbursement Arrangements (ICHRAs). Rebranded as Custom Health Option and Individual Care Expense (CHOICE) Arrangements, these updates codify and enhance ICHRA, offering employers and employees greater flexibility and tax advantages. Below, we explore the key changes and how employers are leveraging them to optimize health benefits.
Key Changes to ICHRA Under the OBBBA
Understanding the New ICHRA Rules Under the One Big Beautiful Bill Act: A Game-Changer for Employers
The One Big Beautiful Bill Act (OBBBA), signed into law on July 4, 2025, has brought significant changes to employee benefits, including updates to Individual Coverage Health Reimbursement Arrangements (ICHRAs). Rebranded as Custom Health Option and Individual Care Expense (CHOICE) Arrangements, these updates codify and enhance ICHRA, offering employers and employees greater flexibility and tax advantages. Below, we explore the key changes and how employers are leveraging them to optimize health benefits.
Key Changes to ICHRA Under the OBBBA
- Codification into Law: Previously operating under 2019 regulatory guidance, ICHRAs are now formalized as CHOICE Arrangements in federal law, ensuring long-term stability regardless of administrative changes. This gives employers confidence in adopting and maintaining these plans.
- Increased Flexibility for Small Employers: Small businesses (fewer than 50 employees) can now offer both CHOICE Arrangements and traditional group health plans to the same employee class, a significant shift from previous restrictions. This allows tailored benefits strategies, such as offering part-time workers a CHOICE Arrangement while providing salaried employees a group plan.
- Pre-Tax Premium Payments: Employees can now pay their share of individual health insurance premiums (including ACA Marketplace plans) on a pre-tax basis through Section 125 cafeteria plans. This change enhances affordability for employees and simplifies administration for employers.
- Small Business Tax Credits: The OBBBA introduces a two-year tax credit for small businesses: $100 per employee per month in the first year and $50 per month in the second year. This incentive encourages adoption among smaller employers, making health benefits more accessible.
- Reduced Notice Period: The required notice period for informing employees about CHOICE Arrangements has been shortened from 90 days to 60 days, easing administrative burdens and allowing faster implementation.
- W-2 Reporting Requirement: Employers must now include the CHOICE Arrangement amount on employees' Form W-2, improving transparency and compliance.
- Employers are embracing CHOICE Arrangements for their flexibility, cost control, and employee satisfaction benefits. Here's how:
- Cost Management: Unlike traditional group health plans, CHOICE Arrangements allow employers to set a fixed budget for health benefits, avoiding unpredictable premium increases. This is particularly appealing to small and midsize businesses seeking cost-effective alternatives.
- Employee Choice and Satisfaction: Employees can select individual health plans that best fit their needs, from ACA Marketplace options to off-exchange plans. This personalization enhances employee satisfaction and helps attract talent in competitive markets.
- Tax Advantages: The ability to offer pre-tax premium payments and the new tax credits for small businesses make CHOICE Arrangements financially attractive. Employers can provide robust benefits while reducing tax liabilities.
Scalability Across Business Sizes: With no size restrictions or contribution caps, CHOICE Arrangements are scalable for businesses of all sizes, from startups to large corporations. This flexibility supports diverse workforce needs, such as varying allowances for full-time, part-time, or seasonal employees. Compliance with ACA: CHOICE Arrangements help employers meet Affordable Care Act (ACA) mandates by ensuring affordability (premiums not exceeding 9.02% of household income for self-only coverage). Employers can design plans to avoid penalties while offering employees access to Marketplace subsidies if needed.
2025 ACA & Medicaid Changes: What You Need to Know
Sunday, July 6, 2025 1 Stop Benefits, Inc.
 Big changes to health insurance rules are here-and many people could lose coverage if they don't act. We're here to make sure that's not you.
No More Auto-Renewals
What this means:
If you have an ACA Marketplace plan, you'll now need to re-apply every year. No more automatic re-enrollment.
What to do:
Big changes to health insurance rules are here-and many people could lose coverage if they don't act. We're here to make sure that's not you.
No More Auto-Renewals
What this means:
If you have an ACA Marketplace plan, you'll now need to re-apply every year. No more automatic re-enrollment.
What to do:
 Big changes to health insurance rules are here-and many people could lose coverage if they don't act. We're here to make sure that's not you.
No More Auto-Renewals
What this means:
If you have an ACA Marketplace plan, you'll now need to re-apply every year. No more automatic re-enrollment.
What to do:
Big changes to health insurance rules are here-and many people could lose coverage if they don't act. We're here to make sure that's not you.
No More Auto-Renewals
What this means:
If you have an ACA Marketplace plan, you'll now need to re-apply every year. No more automatic re-enrollment.
What to do:
- Mark your calendar for the shorter Open Enrollment period.
- Work with us early-we'll make sure your application is submitted on time and with all documentation.
- Be ready to show pay stubs, tax info, or other documents during the year.
- Let us help with gathering and uploading your documents.
- Let us shop all available options-Marketplace, off-Marketplace, short-term, or employer alternatives.
- Ask about bundling dental, vision, or enhanced life and long-term care benefits.
- Check if you qualify for an exemption (health, caregiving, student status).
- We'll help track and report work hours or file exemption paperwork.
- We can explore affordable private options that don't rely on ACA subsidies.
- Ask us about guaranteed issue and low-premium limited benefit plans.
Part-Time Surveys, Full-Time Health Benefits: A Smarter Way to Get Covered
Wednesday, April 10, 2025 Craig Chapin
 In today's evolving healthcare environment, innovative programs are reshaping how individuals access meaningful, affordable coverage. LifeX and Population Science Management (PSM) are leading the charge by offering a unique model: contribute to public health research through short, part-time surveys-and in return, gain access to comprehensive group health insurance.
How It Works
Both companies hire individuals as part-time associates to complete occasional surveys- each typically taking just 5 to 10 minutes, with only a few hours required over the course of a year. Participants are paid for their time and, more importantly, gain access to high-quality, off-exchange health insurance plans.
At 1 Stop Benefits, Inc., we're proud to serve as a recruiting partner for these programs, connecting individuals with this smart, impactful opportunity. It's a win-win: contribute to better public health while securing valuable coverage for yourself and your family.
In today's evolving healthcare environment, innovative programs are reshaping how individuals access meaningful, affordable coverage. LifeX and Population Science Management (PSM) are leading the charge by offering a unique model: contribute to public health research through short, part-time surveys-and in return, gain access to comprehensive group health insurance.
How It Works
Both companies hire individuals as part-time associates to complete occasional surveys- each typically taking just 5 to 10 minutes, with only a few hours required over the course of a year. Participants are paid for their time and, more importantly, gain access to high-quality, off-exchange health insurance plans.
At 1 Stop Benefits, Inc., we're proud to serve as a recruiting partner for these programs, connecting individuals with this smart, impactful opportunity. It's a win-win: contribute to better public health while securing valuable coverage for yourself and your family.
Highlights of Off-Exchange Group Health Plans
Ready to learn more or see if you qualify? Reach out to 1 Stop Benefits today-we're happy to walk you through your options and answer any questions, with no pressure. Call us at 1-800-662-3982 or email: info@1StopBenefits.com to get started.
Highlights of Off-Exchange Group Health Plans
- Flexible Plan Options -- Choose from a range of deductibles and coverage levels
- Great for High Earners -- Ideal for those ineligible for ACA subsidies
- Eligibility -- Available to 1099 contractors, self-employed professionals, and non-working individuals under age 65
By classifying survey participants as part-time associates, LifeX and PSM can offer group health plans-making comprehensive insurance accessible to more people, especially those who fall through the cracks of traditional systems.
- No Balance Billing -- Pre-negotiated rates help reduce unexpected costs
- Lower Shared Expenses -- In-network care keeps your out-of-pocket costs down
- Comprehensive Benefits -- Includes telehealth, pharmacy coverage, and chronic care support
- Freedom of Access -- Nationwide networks with no referrals required
- LifeX -- Tiered premiums with access to PHCS, Cigna, and Anthem
- PSM -- Nationwide access via Blue Cross Blue Shield and PHCS
- Health Surveys + EHRs -- Combine insights for a full picture of health trends
- Predictive Analytics -- Identify emerging risks and support early intervention
- Personalized Solutions -- Tailor strategies to improve community health outcomes
Ready to learn more or see if you qualify? Reach out to 1 Stop Benefits today-we're happy to walk you through your options and answer any questions, with no pressure. Call us at 1-800-662-3982 or email: info@1StopBenefits.com to get started.
Two Plans Are Better Than One
Monday, August 21, 2023 Craig E Chapin
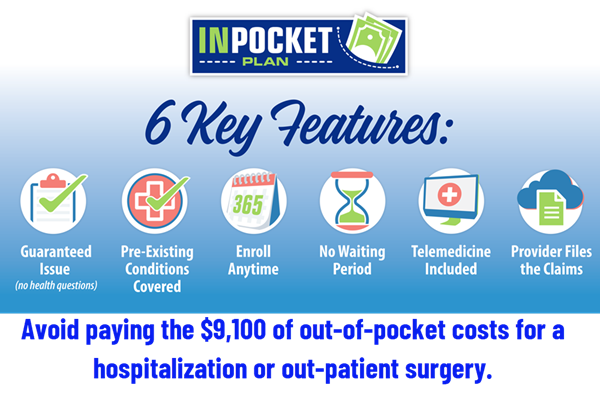
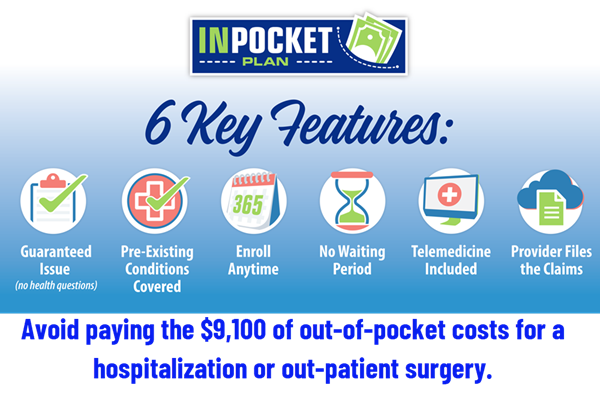 In an ever-changing healthcare landscape, arming yourself with knowledge about health insurance is vital not only for your physical health but also for your financial security. A new insurance plan offers relief to individuals covered by Affordable Care individual health plans regardless of medical conditions and without the standard exclusions. Now, having two insurance plans provides lower out-of-pocket costs than one. The MOOP (maximum out-of-pocket) expenses will be $9,200 per individual and $18,400 per family 2025. Tiered health plans can speed up your obligations. Start saving or read on.
In the insurance industry, one thing remains consistent. 20% of people use 80% of healthcare expenses. Since the Obama Care began, individuals have been insured regardless of their pre-existing conditions or medical expenses. Premium costs have been increasing every year since the law was passed. However, for many participants, the actual premium cost is not obvious as the subsidies granted by the Affordable Care Act offset the increases. What is apparent is that the out-of-pocket costs are increasing and are unaffordable for the average family.
For many, hospital indemnity insurance plans fill the gap for a fraction of the cost of buying up to gold health plans. However, not all states allow hospital indemnity plans to be offered to individuals. Most do not cover the significant upfront costs on the first day in the hospital, and few cover outpatient surgeries. Most are also unavailable to people with pre-existing conditions, and just about all do not cover maternity and mental health expenses.
Life happens, and everyone needs to set up an emergency fund or leverage their limited funds. Solutions now exist to cover your medical bills for accidents only or both sickness and accidents. Do the math to save money by comparing the MOOP and premiums on bronze, silver, and gold individual health plans. People covered by tiered networks (i.e., Proactive Plans) must understand that an ambulance takes you to the nearest hospital regardless of tier status or network. (St Mary's is Tier 3 with Keystone Proactive Plans). Consider lowering your out-of-pocket costs for families planning on more children or baby boomers with a higher risk of hospitalization. Sleep better knowing you can afford to be taken to the nearest hospital or get treated without the risk of medical bankruptcy.
In an ever-changing healthcare landscape, arming yourself with knowledge about health insurance is vital not only for your physical health but also for your financial security. A new insurance plan offers relief to individuals covered by Affordable Care individual health plans regardless of medical conditions and without the standard exclusions. Now, having two insurance plans provides lower out-of-pocket costs than one. The MOOP (maximum out-of-pocket) expenses will be $9,200 per individual and $18,400 per family 2025. Tiered health plans can speed up your obligations. Start saving or read on.
In the insurance industry, one thing remains consistent. 20% of people use 80% of healthcare expenses. Since the Obama Care began, individuals have been insured regardless of their pre-existing conditions or medical expenses. Premium costs have been increasing every year since the law was passed. However, for many participants, the actual premium cost is not obvious as the subsidies granted by the Affordable Care Act offset the increases. What is apparent is that the out-of-pocket costs are increasing and are unaffordable for the average family.
For many, hospital indemnity insurance plans fill the gap for a fraction of the cost of buying up to gold health plans. However, not all states allow hospital indemnity plans to be offered to individuals. Most do not cover the significant upfront costs on the first day in the hospital, and few cover outpatient surgeries. Most are also unavailable to people with pre-existing conditions, and just about all do not cover maternity and mental health expenses.
Life happens, and everyone needs to set up an emergency fund or leverage their limited funds. Solutions now exist to cover your medical bills for accidents only or both sickness and accidents. Do the math to save money by comparing the MOOP and premiums on bronze, silver, and gold individual health plans. People covered by tiered networks (i.e., Proactive Plans) must understand that an ambulance takes you to the nearest hospital regardless of tier status or network. (St Mary's is Tier 3 with Keystone Proactive Plans). Consider lowering your out-of-pocket costs for families planning on more children or baby boomers with a higher risk of hospitalization. Sleep better knowing you can afford to be taken to the nearest hospital or get treated without the risk of medical bankruptcy.
 In an ever-changing healthcare landscape, arming yourself with knowledge about health insurance is vital not only for your physical health but also for your financial security. A new insurance plan offers relief to individuals covered by Affordable Care individual health plans regardless of medical conditions and without the standard exclusions. Now, having two insurance plans provides lower out-of-pocket costs than one. The MOOP (maximum out-of-pocket) expenses will be $9,200 per individual and $18,400 per family 2025. Tiered health plans can speed up your obligations. Start saving or read on.
In the insurance industry, one thing remains consistent. 20% of people use 80% of healthcare expenses. Since the Obama Care began, individuals have been insured regardless of their pre-existing conditions or medical expenses. Premium costs have been increasing every year since the law was passed. However, for many participants, the actual premium cost is not obvious as the subsidies granted by the Affordable Care Act offset the increases. What is apparent is that the out-of-pocket costs are increasing and are unaffordable for the average family.
For many, hospital indemnity insurance plans fill the gap for a fraction of the cost of buying up to gold health plans. However, not all states allow hospital indemnity plans to be offered to individuals. Most do not cover the significant upfront costs on the first day in the hospital, and few cover outpatient surgeries. Most are also unavailable to people with pre-existing conditions, and just about all do not cover maternity and mental health expenses.
Life happens, and everyone needs to set up an emergency fund or leverage their limited funds. Solutions now exist to cover your medical bills for accidents only or both sickness and accidents. Do the math to save money by comparing the MOOP and premiums on bronze, silver, and gold individual health plans. People covered by tiered networks (i.e., Proactive Plans) must understand that an ambulance takes you to the nearest hospital regardless of tier status or network. (St Mary's is Tier 3 with Keystone Proactive Plans). Consider lowering your out-of-pocket costs for families planning on more children or baby boomers with a higher risk of hospitalization. Sleep better knowing you can afford to be taken to the nearest hospital or get treated without the risk of medical bankruptcy.
In an ever-changing healthcare landscape, arming yourself with knowledge about health insurance is vital not only for your physical health but also for your financial security. A new insurance plan offers relief to individuals covered by Affordable Care individual health plans regardless of medical conditions and without the standard exclusions. Now, having two insurance plans provides lower out-of-pocket costs than one. The MOOP (maximum out-of-pocket) expenses will be $9,200 per individual and $18,400 per family 2025. Tiered health plans can speed up your obligations. Start saving or read on.
In the insurance industry, one thing remains consistent. 20% of people use 80% of healthcare expenses. Since the Obama Care began, individuals have been insured regardless of their pre-existing conditions or medical expenses. Premium costs have been increasing every year since the law was passed. However, for many participants, the actual premium cost is not obvious as the subsidies granted by the Affordable Care Act offset the increases. What is apparent is that the out-of-pocket costs are increasing and are unaffordable for the average family.
For many, hospital indemnity insurance plans fill the gap for a fraction of the cost of buying up to gold health plans. However, not all states allow hospital indemnity plans to be offered to individuals. Most do not cover the significant upfront costs on the first day in the hospital, and few cover outpatient surgeries. Most are also unavailable to people with pre-existing conditions, and just about all do not cover maternity and mental health expenses.
Life happens, and everyone needs to set up an emergency fund or leverage their limited funds. Solutions now exist to cover your medical bills for accidents only or both sickness and accidents. Do the math to save money by comparing the MOOP and premiums on bronze, silver, and gold individual health plans. People covered by tiered networks (i.e., Proactive Plans) must understand that an ambulance takes you to the nearest hospital regardless of tier status or network. (St Mary's is Tier 3 with Keystone Proactive Plans). Consider lowering your out-of-pocket costs for families planning on more children or baby boomers with a higher risk of hospitalization. Sleep better knowing you can afford to be taken to the nearest hospital or get treated without the risk of medical bankruptcy.
Updates to Medicare Part D Medication Coverage
Tuesday, July 18, 2023 Craig E Chapin
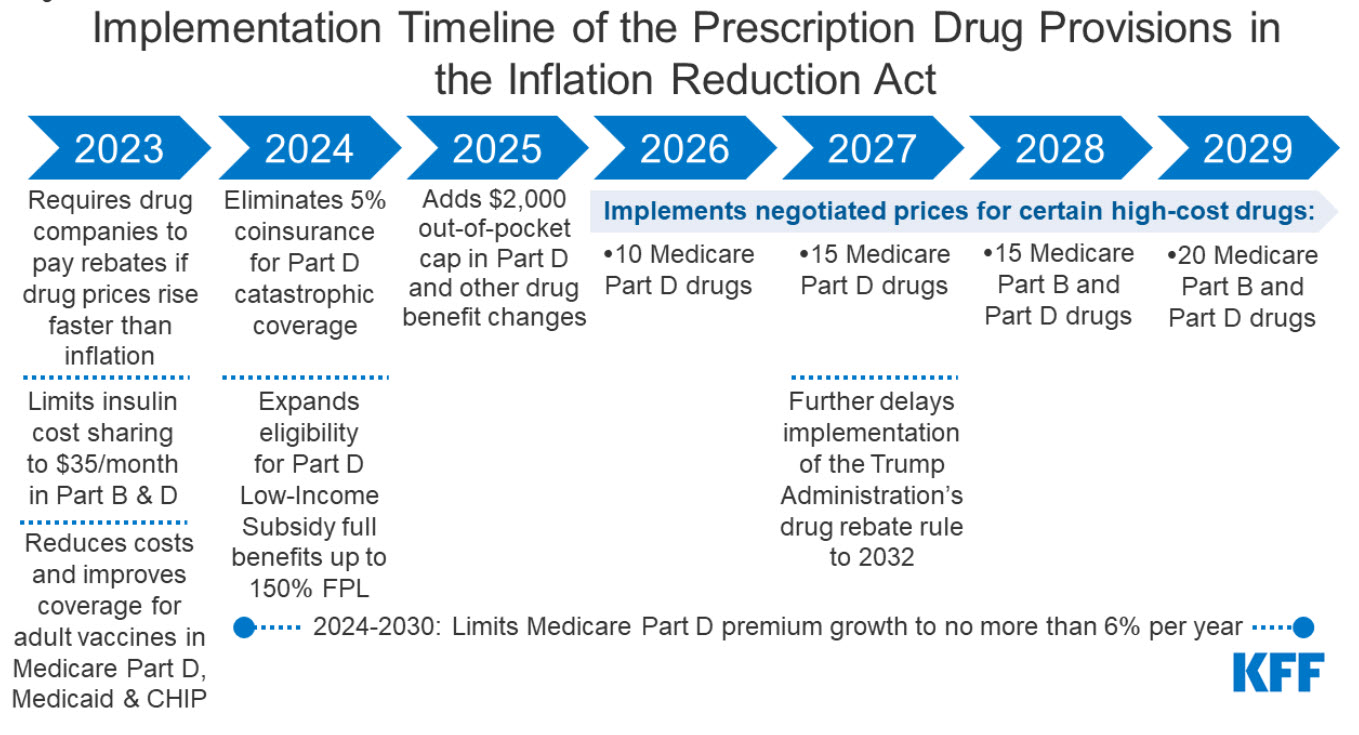
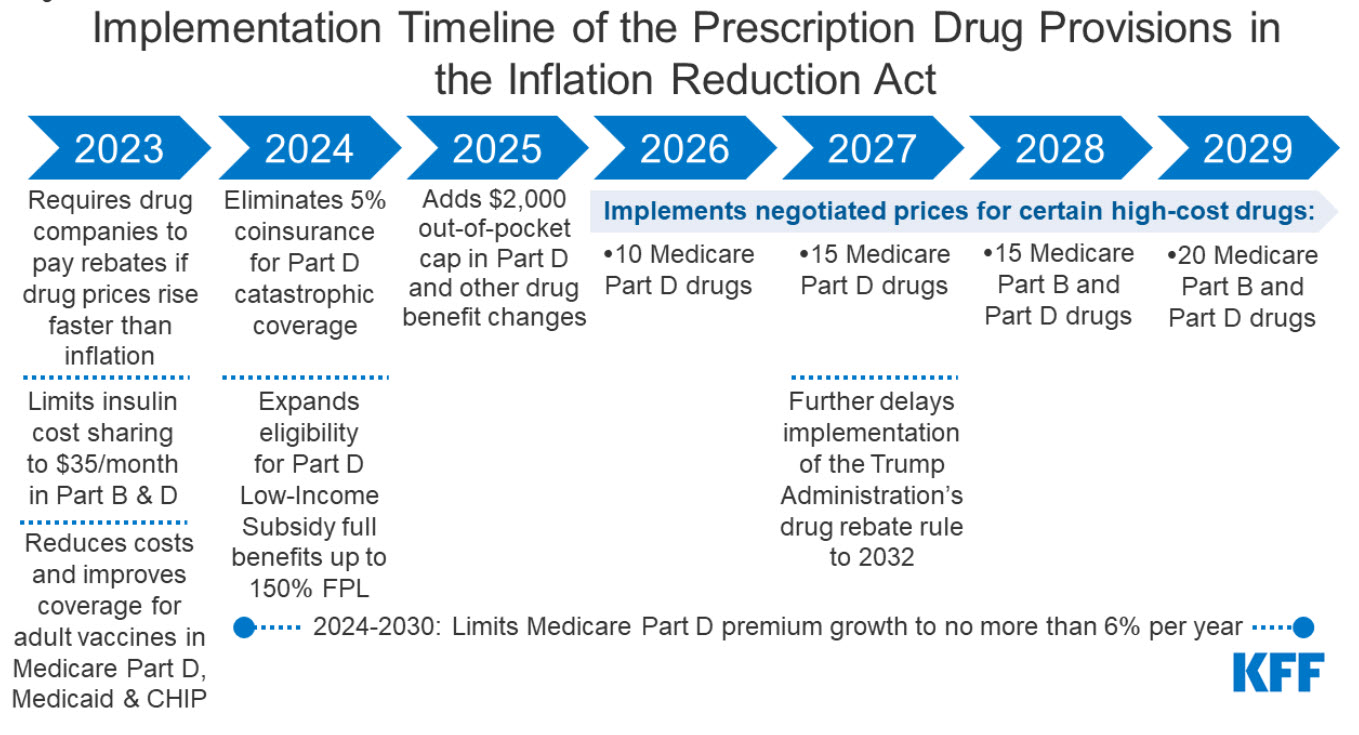 Staying informed about changes to Medicare Part D medication coverage is essential for understanding how these updates may impact healthcare expenses and treatment options. This blog post will explore the recent Medicare Part D medication coverage improvements that the Infl initiated by the Inflation Reduction Act.
1. The law requires the federal government to negotiate prices for some high-cost drugs covered under Medicare. Medicare Part D and Part B drug spending are highly concentrated among a relatively small share of covered drugs, mainly those without generic or biosimilar competitors. Under the Inflation Reduction Act, brand-name and biologic drugs without generic or biosimilar equivalents covered under Medicare Part D that are among the highest-spending Medicare-covered drugs are eligible for negotiation. The number of negotiated drugs is limited to 10 Part D drugs in 2026, another 15 Part D drugs in 2027, another 15 Part B and Part D drugs in 2028, and another 20 Part B and Part D drugs in 2029 and later years.
2. The law requires drug manufacturers to pay Medicare rebates if they increase prices faster than inflation for drugs used by Medicare beneficiaries. The inflation rebate provision will be implemented in 2023, using 2021 as the base year for determining price changes relative to inflation.
3. The law Caps Medicare beneficiaries' out-of-pocket spending under the Medicare Part D benefit, first eliminating coinsurance above the catastrophic threshold in 2024 and then adding a $2,000 cap on spending in 2025. It also limits annual increases in Part D premiums from 2024 to 2030 and makes other changes to the Part D benefit design.
4. Beginning in 2023, the bill limits cost-sharing for insulin to $35 per month for people with Medicare, including covered insulin products in Medicare Part D plans, beginning January 1, 2023, and for insulin furnished through durable medical equipment under Medicare Part B, starting July 1, 2023.
5. Eliminates cost-sharing for adult vaccines covered under Medicare Part D, as of 2023, and improves access to adult vaccines under Medicaid and CHIP.
6. It expands eligibility for full Part D Low-Income Subsidies (LIS) in 2024 to low-income beneficiaries with incomes up to 150% of poverty and modest assets and repeals the partial LIS benefit currently in place for individuals with incomes between 135% and 150% of poverty.
7. Expanded Medication Therapy Management (MTM) Services: MTM services have been expanded to provide enhanced support and guidance. This helps ensure effective medication use, improves health outcomes, and minimizes drug-related issues.
8. Enhanced Information and Decision-Making Tools: Beneficiaries now have improved resources for informed decision-making. The updated Plan Finder tool offers accurate cost estimates and helps select the most suitable Part D plan based on individual medication needs.
Conclusion: Staying updated on Medicare Part D medication coverage changes is crucial for beneficiaries seeking affordable and necessary prescription drugs. Recent enhancements, including improved coverage in the donut hole, biosimilar discounts, expanded catastrophic coverage threshold, expanded MTM services, and enhanced information tools, contribute to greater affordability and accessibility. Beneficiaries are encouraged to remain informed, review their Part D plan regularly, and utilize available resources to make informed decisions about prescription drug coverage.
Disclaimer: The information provided is for educational purposes only and not legal or financial advice. Consult a qualified professional for personalized guidance regarding your specific situation.
Staying informed about changes to Medicare Part D medication coverage is essential for understanding how these updates may impact healthcare expenses and treatment options. This blog post will explore the recent Medicare Part D medication coverage improvements that the Infl initiated by the Inflation Reduction Act.
1. The law requires the federal government to negotiate prices for some high-cost drugs covered under Medicare. Medicare Part D and Part B drug spending are highly concentrated among a relatively small share of covered drugs, mainly those without generic or biosimilar competitors. Under the Inflation Reduction Act, brand-name and biologic drugs without generic or biosimilar equivalents covered under Medicare Part D that are among the highest-spending Medicare-covered drugs are eligible for negotiation. The number of negotiated drugs is limited to 10 Part D drugs in 2026, another 15 Part D drugs in 2027, another 15 Part B and Part D drugs in 2028, and another 20 Part B and Part D drugs in 2029 and later years.
2. The law requires drug manufacturers to pay Medicare rebates if they increase prices faster than inflation for drugs used by Medicare beneficiaries. The inflation rebate provision will be implemented in 2023, using 2021 as the base year for determining price changes relative to inflation.
3. The law Caps Medicare beneficiaries' out-of-pocket spending under the Medicare Part D benefit, first eliminating coinsurance above the catastrophic threshold in 2024 and then adding a $2,000 cap on spending in 2025. It also limits annual increases in Part D premiums from 2024 to 2030 and makes other changes to the Part D benefit design.
4. Beginning in 2023, the bill limits cost-sharing for insulin to $35 per month for people with Medicare, including covered insulin products in Medicare Part D plans, beginning January 1, 2023, and for insulin furnished through durable medical equipment under Medicare Part B, starting July 1, 2023.
5. Eliminates cost-sharing for adult vaccines covered under Medicare Part D, as of 2023, and improves access to adult vaccines under Medicaid and CHIP.
6. It expands eligibility for full Part D Low-Income Subsidies (LIS) in 2024 to low-income beneficiaries with incomes up to 150% of poverty and modest assets and repeals the partial LIS benefit currently in place for individuals with incomes between 135% and 150% of poverty.
7. Expanded Medication Therapy Management (MTM) Services: MTM services have been expanded to provide enhanced support and guidance. This helps ensure effective medication use, improves health outcomes, and minimizes drug-related issues.
8. Enhanced Information and Decision-Making Tools: Beneficiaries now have improved resources for informed decision-making. The updated Plan Finder tool offers accurate cost estimates and helps select the most suitable Part D plan based on individual medication needs.
Conclusion: Staying updated on Medicare Part D medication coverage changes is crucial for beneficiaries seeking affordable and necessary prescription drugs. Recent enhancements, including improved coverage in the donut hole, biosimilar discounts, expanded catastrophic coverage threshold, expanded MTM services, and enhanced information tools, contribute to greater affordability and accessibility. Beneficiaries are encouraged to remain informed, review their Part D plan regularly, and utilize available resources to make informed decisions about prescription drug coverage.
Disclaimer: The information provided is for educational purposes only and not legal or financial advice. Consult a qualified professional for personalized guidance regarding your specific situation.
 Staying informed about changes to Medicare Part D medication coverage is essential for understanding how these updates may impact healthcare expenses and treatment options. This blog post will explore the recent Medicare Part D medication coverage improvements that the Infl initiated by the Inflation Reduction Act.
1. The law requires the federal government to negotiate prices for some high-cost drugs covered under Medicare. Medicare Part D and Part B drug spending are highly concentrated among a relatively small share of covered drugs, mainly those without generic or biosimilar competitors. Under the Inflation Reduction Act, brand-name and biologic drugs without generic or biosimilar equivalents covered under Medicare Part D that are among the highest-spending Medicare-covered drugs are eligible for negotiation. The number of negotiated drugs is limited to 10 Part D drugs in 2026, another 15 Part D drugs in 2027, another 15 Part B and Part D drugs in 2028, and another 20 Part B and Part D drugs in 2029 and later years.
2. The law requires drug manufacturers to pay Medicare rebates if they increase prices faster than inflation for drugs used by Medicare beneficiaries. The inflation rebate provision will be implemented in 2023, using 2021 as the base year for determining price changes relative to inflation.
3. The law Caps Medicare beneficiaries' out-of-pocket spending under the Medicare Part D benefit, first eliminating coinsurance above the catastrophic threshold in 2024 and then adding a $2,000 cap on spending in 2025. It also limits annual increases in Part D premiums from 2024 to 2030 and makes other changes to the Part D benefit design.
4. Beginning in 2023, the bill limits cost-sharing for insulin to $35 per month for people with Medicare, including covered insulin products in Medicare Part D plans, beginning January 1, 2023, and for insulin furnished through durable medical equipment under Medicare Part B, starting July 1, 2023.
5. Eliminates cost-sharing for adult vaccines covered under Medicare Part D, as of 2023, and improves access to adult vaccines under Medicaid and CHIP.
6. It expands eligibility for full Part D Low-Income Subsidies (LIS) in 2024 to low-income beneficiaries with incomes up to 150% of poverty and modest assets and repeals the partial LIS benefit currently in place for individuals with incomes between 135% and 150% of poverty.
7. Expanded Medication Therapy Management (MTM) Services: MTM services have been expanded to provide enhanced support and guidance. This helps ensure effective medication use, improves health outcomes, and minimizes drug-related issues.
8. Enhanced Information and Decision-Making Tools: Beneficiaries now have improved resources for informed decision-making. The updated Plan Finder tool offers accurate cost estimates and helps select the most suitable Part D plan based on individual medication needs.
Conclusion: Staying updated on Medicare Part D medication coverage changes is crucial for beneficiaries seeking affordable and necessary prescription drugs. Recent enhancements, including improved coverage in the donut hole, biosimilar discounts, expanded catastrophic coverage threshold, expanded MTM services, and enhanced information tools, contribute to greater affordability and accessibility. Beneficiaries are encouraged to remain informed, review their Part D plan regularly, and utilize available resources to make informed decisions about prescription drug coverage.
Disclaimer: The information provided is for educational purposes only and not legal or financial advice. Consult a qualified professional for personalized guidance regarding your specific situation.
Staying informed about changes to Medicare Part D medication coverage is essential for understanding how these updates may impact healthcare expenses and treatment options. This blog post will explore the recent Medicare Part D medication coverage improvements that the Infl initiated by the Inflation Reduction Act.
1. The law requires the federal government to negotiate prices for some high-cost drugs covered under Medicare. Medicare Part D and Part B drug spending are highly concentrated among a relatively small share of covered drugs, mainly those without generic or biosimilar competitors. Under the Inflation Reduction Act, brand-name and biologic drugs without generic or biosimilar equivalents covered under Medicare Part D that are among the highest-spending Medicare-covered drugs are eligible for negotiation. The number of negotiated drugs is limited to 10 Part D drugs in 2026, another 15 Part D drugs in 2027, another 15 Part B and Part D drugs in 2028, and another 20 Part B and Part D drugs in 2029 and later years.
2. The law requires drug manufacturers to pay Medicare rebates if they increase prices faster than inflation for drugs used by Medicare beneficiaries. The inflation rebate provision will be implemented in 2023, using 2021 as the base year for determining price changes relative to inflation.
3. The law Caps Medicare beneficiaries' out-of-pocket spending under the Medicare Part D benefit, first eliminating coinsurance above the catastrophic threshold in 2024 and then adding a $2,000 cap on spending in 2025. It also limits annual increases in Part D premiums from 2024 to 2030 and makes other changes to the Part D benefit design.
4. Beginning in 2023, the bill limits cost-sharing for insulin to $35 per month for people with Medicare, including covered insulin products in Medicare Part D plans, beginning January 1, 2023, and for insulin furnished through durable medical equipment under Medicare Part B, starting July 1, 2023.
5. Eliminates cost-sharing for adult vaccines covered under Medicare Part D, as of 2023, and improves access to adult vaccines under Medicaid and CHIP.
6. It expands eligibility for full Part D Low-Income Subsidies (LIS) in 2024 to low-income beneficiaries with incomes up to 150% of poverty and modest assets and repeals the partial LIS benefit currently in place for individuals with incomes between 135% and 150% of poverty.
7. Expanded Medication Therapy Management (MTM) Services: MTM services have been expanded to provide enhanced support and guidance. This helps ensure effective medication use, improves health outcomes, and minimizes drug-related issues.
8. Enhanced Information and Decision-Making Tools: Beneficiaries now have improved resources for informed decision-making. The updated Plan Finder tool offers accurate cost estimates and helps select the most suitable Part D plan based on individual medication needs.
Conclusion: Staying updated on Medicare Part D medication coverage changes is crucial for beneficiaries seeking affordable and necessary prescription drugs. Recent enhancements, including improved coverage in the donut hole, biosimilar discounts, expanded catastrophic coverage threshold, expanded MTM services, and enhanced information tools, contribute to greater affordability and accessibility. Beneficiaries are encouraged to remain informed, review their Part D plan regularly, and utilize available resources to make informed decisions about prescription drug coverage.
Disclaimer: The information provided is for educational purposes only and not legal or financial advice. Consult a qualified professional for personalized guidance regarding your specific situation.
NJ is making a mistake by robbing the group health market to pay for the NJHPTC.
Thursday, March 24, 2023 Craig E Chapin, Pesident
 Using NJ state and federal subsidies, the Affordable Care Act (ACA) helps eligible individuals and families afford health insurance. The American Rescue Plan Act has increased the amount of financial help available, with no one paying more than 8.5% of their income for health insurance when not offered affordable group health insurance through work. New Jersey has its own subsidy program, the New Jersey Health Insurance Premium Tax Credit (NJHPTC), funded by state taxes, fees, and assessments on health insurance companies and hospitals, as well as the state's general fund. However, NJ added subsidy may cause small employers to stop offering group health plans.
To be eligible for NJHPTC, individuals, and families must meet certain income requirements, and the amount of subsidy varies based on the number of insured individuals. For example, an individual making 150% of the Federal Poverty Level will receive combined subsidies, making many health plans have zero premiums. Adults making less than 401% of the FPL get an extra $100 a month, and incomes between 401% to 600% of the FPL will get $50 a month.
Children dependents under age 19 default to the Children's Health Insurance Program at zero cost if the household earns less than 355% of the FPL. The adults receive the NJHPTC as indicated above. If the child is over 18, they are treated as an adult, getting up to an additional $100 credit per child under 400% of the FPL and $50 from 401% up to 600% of the FPL.
The CHIP insures over one million children in NJ, and growing the pool is a priority to move to a one-payer system. To avoid a child's eligibility for CHIP, the family must report an income over 355% of the FPL, or they can refuse the free coverage and enroll their children in a non-subsidized plan through the same insurance companies offered to adults. The Child Health Insurance Program offers comprehensive coverage, including dental and vision.
When a state takes funds from the health industry and hospitals to fund the subsidy, insurance companies and hospitals will pass the cost on to all users, increasing the overall cost. Eventually, as small group premiums increase, many employers will stop offering group coverage and direct employees to purchase subsidized individual plans. The Family Glitch Fix will further enlighten employers about how little individuals pay for health insurance. The fix allows dependents of employees covered by group health plans to enroll in subsidized individual health plans if the household cost is determined unaffordable. Groups under 50 employees do not have a penalty for not offering health insurance, so when the cost can be sliced in half, an employer's premium contributions may be better allocated to other benefits or an increase in pay.
The subsidy programs aim to balance the cost burden across different groups, with the hope that increased access to healthcare will ultimately lead to better health outcomes and lower overall healthcare costs in the long run. With over forty years of experience, I feel usage will increase, moral hazard will not lead to better healthcare outcomes, and participants will demand the entitlement to be maintained while others pay the cost.
Using NJ state and federal subsidies, the Affordable Care Act (ACA) helps eligible individuals and families afford health insurance. The American Rescue Plan Act has increased the amount of financial help available, with no one paying more than 8.5% of their income for health insurance when not offered affordable group health insurance through work. New Jersey has its own subsidy program, the New Jersey Health Insurance Premium Tax Credit (NJHPTC), funded by state taxes, fees, and assessments on health insurance companies and hospitals, as well as the state's general fund. However, NJ added subsidy may cause small employers to stop offering group health plans.
To be eligible for NJHPTC, individuals, and families must meet certain income requirements, and the amount of subsidy varies based on the number of insured individuals. For example, an individual making 150% of the Federal Poverty Level will receive combined subsidies, making many health plans have zero premiums. Adults making less than 401% of the FPL get an extra $100 a month, and incomes between 401% to 600% of the FPL will get $50 a month.
Children dependents under age 19 default to the Children's Health Insurance Program at zero cost if the household earns less than 355% of the FPL. The adults receive the NJHPTC as indicated above. If the child is over 18, they are treated as an adult, getting up to an additional $100 credit per child under 400% of the FPL and $50 from 401% up to 600% of the FPL.
The CHIP insures over one million children in NJ, and growing the pool is a priority to move to a one-payer system. To avoid a child's eligibility for CHIP, the family must report an income over 355% of the FPL, or they can refuse the free coverage and enroll their children in a non-subsidized plan through the same insurance companies offered to adults. The Child Health Insurance Program offers comprehensive coverage, including dental and vision.
When a state takes funds from the health industry and hospitals to fund the subsidy, insurance companies and hospitals will pass the cost on to all users, increasing the overall cost. Eventually, as small group premiums increase, many employers will stop offering group coverage and direct employees to purchase subsidized individual plans. The Family Glitch Fix will further enlighten employers about how little individuals pay for health insurance. The fix allows dependents of employees covered by group health plans to enroll in subsidized individual health plans if the household cost is determined unaffordable. Groups under 50 employees do not have a penalty for not offering health insurance, so when the cost can be sliced in half, an employer's premium contributions may be better allocated to other benefits or an increase in pay.
The subsidy programs aim to balance the cost burden across different groups, with the hope that increased access to healthcare will ultimately lead to better health outcomes and lower overall healthcare costs in the long run. With over forty years of experience, I feel usage will increase, moral hazard will not lead to better healthcare outcomes, and participants will demand the entitlement to be maintained while others pay the cost.
 Using NJ state and federal subsidies, the Affordable Care Act (ACA) helps eligible individuals and families afford health insurance. The American Rescue Plan Act has increased the amount of financial help available, with no one paying more than 8.5% of their income for health insurance when not offered affordable group health insurance through work. New Jersey has its own subsidy program, the New Jersey Health Insurance Premium Tax Credit (NJHPTC), funded by state taxes, fees, and assessments on health insurance companies and hospitals, as well as the state's general fund. However, NJ added subsidy may cause small employers to stop offering group health plans.
To be eligible for NJHPTC, individuals, and families must meet certain income requirements, and the amount of subsidy varies based on the number of insured individuals. For example, an individual making 150% of the Federal Poverty Level will receive combined subsidies, making many health plans have zero premiums. Adults making less than 401% of the FPL get an extra $100 a month, and incomes between 401% to 600% of the FPL will get $50 a month.
Children dependents under age 19 default to the Children's Health Insurance Program at zero cost if the household earns less than 355% of the FPL. The adults receive the NJHPTC as indicated above. If the child is over 18, they are treated as an adult, getting up to an additional $100 credit per child under 400% of the FPL and $50 from 401% up to 600% of the FPL.
The CHIP insures over one million children in NJ, and growing the pool is a priority to move to a one-payer system. To avoid a child's eligibility for CHIP, the family must report an income over 355% of the FPL, or they can refuse the free coverage and enroll their children in a non-subsidized plan through the same insurance companies offered to adults. The Child Health Insurance Program offers comprehensive coverage, including dental and vision.
When a state takes funds from the health industry and hospitals to fund the subsidy, insurance companies and hospitals will pass the cost on to all users, increasing the overall cost. Eventually, as small group premiums increase, many employers will stop offering group coverage and direct employees to purchase subsidized individual plans. The Family Glitch Fix will further enlighten employers about how little individuals pay for health insurance. The fix allows dependents of employees covered by group health plans to enroll in subsidized individual health plans if the household cost is determined unaffordable. Groups under 50 employees do not have a penalty for not offering health insurance, so when the cost can be sliced in half, an employer's premium contributions may be better allocated to other benefits or an increase in pay.
The subsidy programs aim to balance the cost burden across different groups, with the hope that increased access to healthcare will ultimately lead to better health outcomes and lower overall healthcare costs in the long run. With over forty years of experience, I feel usage will increase, moral hazard will not lead to better healthcare outcomes, and participants will demand the entitlement to be maintained while others pay the cost.
Using NJ state and federal subsidies, the Affordable Care Act (ACA) helps eligible individuals and families afford health insurance. The American Rescue Plan Act has increased the amount of financial help available, with no one paying more than 8.5% of their income for health insurance when not offered affordable group health insurance through work. New Jersey has its own subsidy program, the New Jersey Health Insurance Premium Tax Credit (NJHPTC), funded by state taxes, fees, and assessments on health insurance companies and hospitals, as well as the state's general fund. However, NJ added subsidy may cause small employers to stop offering group health plans.
To be eligible for NJHPTC, individuals, and families must meet certain income requirements, and the amount of subsidy varies based on the number of insured individuals. For example, an individual making 150% of the Federal Poverty Level will receive combined subsidies, making many health plans have zero premiums. Adults making less than 401% of the FPL get an extra $100 a month, and incomes between 401% to 600% of the FPL will get $50 a month.
Children dependents under age 19 default to the Children's Health Insurance Program at zero cost if the household earns less than 355% of the FPL. The adults receive the NJHPTC as indicated above. If the child is over 18, they are treated as an adult, getting up to an additional $100 credit per child under 400% of the FPL and $50 from 401% up to 600% of the FPL.
The CHIP insures over one million children in NJ, and growing the pool is a priority to move to a one-payer system. To avoid a child's eligibility for CHIP, the family must report an income over 355% of the FPL, or they can refuse the free coverage and enroll their children in a non-subsidized plan through the same insurance companies offered to adults. The Child Health Insurance Program offers comprehensive coverage, including dental and vision.
When a state takes funds from the health industry and hospitals to fund the subsidy, insurance companies and hospitals will pass the cost on to all users, increasing the overall cost. Eventually, as small group premiums increase, many employers will stop offering group coverage and direct employees to purchase subsidized individual plans. The Family Glitch Fix will further enlighten employers about how little individuals pay for health insurance. The fix allows dependents of employees covered by group health plans to enroll in subsidized individual health plans if the household cost is determined unaffordable. Groups under 50 employees do not have a penalty for not offering health insurance, so when the cost can be sliced in half, an employer's premium contributions may be better allocated to other benefits or an increase in pay.
The subsidy programs aim to balance the cost burden across different groups, with the hope that increased access to healthcare will ultimately lead to better health outcomes and lower overall healthcare costs in the long run. With over forty years of experience, I feel usage will increase, moral hazard will not lead to better healthcare outcomes, and participants will demand the entitlement to be maintained while others pay the cost.
All employees with dependents need to see if the "Family Glitch Fix" applies to them.
Thursday, March 16, 2023
 The "Family Glitch Fix" allows employees with dependent group health coverage to save thousands. Once notified, the fix allows employee dependents denied access to subsidized individual health plans to enroll immediately.
Call us, and we can check affordability in seconds, then calculate your monthly savings in any health plan offered in your area. If your employer offers group health insurance and you have dependents, you may be able to lower your premium costs and their out-of-pocket costs for medical care.
The so-called "family glitch" stems from a 2013 IRS interpretation. Under Section 36B of the Internal Revenue Code, individuals generally do not qualify for premium tax credits if they are eligible for another source of minimum essential coverage, including employer-sponsored plans. There are two exceptions to this rule under the ACA-when the offer of job-based coverage is not "affordable" or not of "minimum value." If either exception is met, an individual is ineligible for minimum essential coverage, making them eligible for premium tax credits.
An employee needs to do this simple test with individual plans less expensive than most group health plans, even without subsidies. With federal and NJ subsidies, the monthly savings are larger than the average car payment.
The "Family Glitch Fix" allows employees with dependent group health coverage to save thousands. Once notified, the fix allows employee dependents denied access to subsidized individual health plans to enroll immediately.
Call us, and we can check affordability in seconds, then calculate your monthly savings in any health plan offered in your area. If your employer offers group health insurance and you have dependents, you may be able to lower your premium costs and their out-of-pocket costs for medical care.
The so-called "family glitch" stems from a 2013 IRS interpretation. Under Section 36B of the Internal Revenue Code, individuals generally do not qualify for premium tax credits if they are eligible for another source of minimum essential coverage, including employer-sponsored plans. There are two exceptions to this rule under the ACA-when the offer of job-based coverage is not "affordable" or not of "minimum value." If either exception is met, an individual is ineligible for minimum essential coverage, making them eligible for premium tax credits.
An employee needs to do this simple test with individual plans less expensive than most group health plans, even without subsidies. With federal and NJ subsidies, the monthly savings are larger than the average car payment.
 The "Family Glitch Fix" allows employees with dependent group health coverage to save thousands. Once notified, the fix allows employee dependents denied access to subsidized individual health plans to enroll immediately.
Call us, and we can check affordability in seconds, then calculate your monthly savings in any health plan offered in your area. If your employer offers group health insurance and you have dependents, you may be able to lower your premium costs and their out-of-pocket costs for medical care.
The so-called "family glitch" stems from a 2013 IRS interpretation. Under Section 36B of the Internal Revenue Code, individuals generally do not qualify for premium tax credits if they are eligible for another source of minimum essential coverage, including employer-sponsored plans. There are two exceptions to this rule under the ACA-when the offer of job-based coverage is not "affordable" or not of "minimum value." If either exception is met, an individual is ineligible for minimum essential coverage, making them eligible for premium tax credits.
An employee needs to do this simple test with individual plans less expensive than most group health plans, even without subsidies. With federal and NJ subsidies, the monthly savings are larger than the average car payment.
The "Family Glitch Fix" allows employees with dependent group health coverage to save thousands. Once notified, the fix allows employee dependents denied access to subsidized individual health plans to enroll immediately.
Call us, and we can check affordability in seconds, then calculate your monthly savings in any health plan offered in your area. If your employer offers group health insurance and you have dependents, you may be able to lower your premium costs and their out-of-pocket costs for medical care.
The so-called "family glitch" stems from a 2013 IRS interpretation. Under Section 36B of the Internal Revenue Code, individuals generally do not qualify for premium tax credits if they are eligible for another source of minimum essential coverage, including employer-sponsored plans. There are two exceptions to this rule under the ACA-when the offer of job-based coverage is not "affordable" or not of "minimum value." If either exception is met, an individual is ineligible for minimum essential coverage, making them eligible for premium tax credits.
An employee needs to do this simple test with individual plans less expensive than most group health plans, even without subsidies. With federal and NJ subsidies, the monthly savings are larger than the average car payment.
What are the best health insurance options for small businesses in 2023
Thursday, February 23, 2023 Craig E Chapin, Pesident
 In 2023, inflation is the central talking point, and health insurance premiums and medical costs are increasing. Small employers must look at benefit costs with salary, and supply costs increasing. If a business offers health insurance, there are three options; Level Funding, Fully Insured, and Individual Health Plans.
Level funding is the new option with reduced premiums and more comprehensive provider access for groups with good claims experience. Health questions are asked, and past medical usage is checked for insurance companies to select groups that are likely to have lower claims expenses than the premiums paid. Groups with as few as two employees can enroll, and the final premium rates remain level for the policy year. Level funding is a great place to start if you want to see if your groups can save while still having the option to fall back on guaranteed, fully insured health plans.
Fully insured plans are changing and offer savings by reducing provider access, especially to out-of-state providers. Many plan designs are moving away from copays on brand name prescriptions and shifting higher cost sharing to employees. The fully insured plans are favored by employers, paying the lion's share of premiums and wanting to offer benefits with little employee involvement.
The small group's health market is yielding to the individual health market that offers rich federal and (NJ State) premium subsidies to employees and cost-sharing reductions on out-of-pocket costs. The Family Glitch law allows dependents for employees covered by group insurance to take advantage of individual subsidies if the employee's cost to insure their dependents is unaffordable. In NJ, the state exploits the small group market by taking premiums and funding individuals not covered by group insurance.
The best program depends on the business's unique needs and its employees. All groups should offer health insurance as employees are also crushed by inflation. Employees need expert advice to take advantage of any offer and will be more productive, resulting in lower absenteeism from financial loss.
In 2023, inflation is the central talking point, and health insurance premiums and medical costs are increasing. Small employers must look at benefit costs with salary, and supply costs increasing. If a business offers health insurance, there are three options; Level Funding, Fully Insured, and Individual Health Plans.
Level funding is the new option with reduced premiums and more comprehensive provider access for groups with good claims experience. Health questions are asked, and past medical usage is checked for insurance companies to select groups that are likely to have lower claims expenses than the premiums paid. Groups with as few as two employees can enroll, and the final premium rates remain level for the policy year. Level funding is a great place to start if you want to see if your groups can save while still having the option to fall back on guaranteed, fully insured health plans.
Fully insured plans are changing and offer savings by reducing provider access, especially to out-of-state providers. Many plan designs are moving away from copays on brand name prescriptions and shifting higher cost sharing to employees. The fully insured plans are favored by employers, paying the lion's share of premiums and wanting to offer benefits with little employee involvement.
The small group's health market is yielding to the individual health market that offers rich federal and (NJ State) premium subsidies to employees and cost-sharing reductions on out-of-pocket costs. The Family Glitch law allows dependents for employees covered by group insurance to take advantage of individual subsidies if the employee's cost to insure their dependents is unaffordable. In NJ, the state exploits the small group market by taking premiums and funding individuals not covered by group insurance.
The best program depends on the business's unique needs and its employees. All groups should offer health insurance as employees are also crushed by inflation. Employees need expert advice to take advantage of any offer and will be more productive, resulting in lower absenteeism from financial loss.
 In 2023, inflation is the central talking point, and health insurance premiums and medical costs are increasing. Small employers must look at benefit costs with salary, and supply costs increasing. If a business offers health insurance, there are three options; Level Funding, Fully Insured, and Individual Health Plans.
Level funding is the new option with reduced premiums and more comprehensive provider access for groups with good claims experience. Health questions are asked, and past medical usage is checked for insurance companies to select groups that are likely to have lower claims expenses than the premiums paid. Groups with as few as two employees can enroll, and the final premium rates remain level for the policy year. Level funding is a great place to start if you want to see if your groups can save while still having the option to fall back on guaranteed, fully insured health plans.
Fully insured plans are changing and offer savings by reducing provider access, especially to out-of-state providers. Many plan designs are moving away from copays on brand name prescriptions and shifting higher cost sharing to employees. The fully insured plans are favored by employers, paying the lion's share of premiums and wanting to offer benefits with little employee involvement.
The small group's health market is yielding to the individual health market that offers rich federal and (NJ State) premium subsidies to employees and cost-sharing reductions on out-of-pocket costs. The Family Glitch law allows dependents for employees covered by group insurance to take advantage of individual subsidies if the employee's cost to insure their dependents is unaffordable. In NJ, the state exploits the small group market by taking premiums and funding individuals not covered by group insurance.
The best program depends on the business's unique needs and its employees. All groups should offer health insurance as employees are also crushed by inflation. Employees need expert advice to take advantage of any offer and will be more productive, resulting in lower absenteeism from financial loss.
In 2023, inflation is the central talking point, and health insurance premiums and medical costs are increasing. Small employers must look at benefit costs with salary, and supply costs increasing. If a business offers health insurance, there are three options; Level Funding, Fully Insured, and Individual Health Plans.
Level funding is the new option with reduced premiums and more comprehensive provider access for groups with good claims experience. Health questions are asked, and past medical usage is checked for insurance companies to select groups that are likely to have lower claims expenses than the premiums paid. Groups with as few as two employees can enroll, and the final premium rates remain level for the policy year. Level funding is a great place to start if you want to see if your groups can save while still having the option to fall back on guaranteed, fully insured health plans.
Fully insured plans are changing and offer savings by reducing provider access, especially to out-of-state providers. Many plan designs are moving away from copays on brand name prescriptions and shifting higher cost sharing to employees. The fully insured plans are favored by employers, paying the lion's share of premiums and wanting to offer benefits with little employee involvement.
The small group's health market is yielding to the individual health market that offers rich federal and (NJ State) premium subsidies to employees and cost-sharing reductions on out-of-pocket costs. The Family Glitch law allows dependents for employees covered by group insurance to take advantage of individual subsidies if the employee's cost to insure their dependents is unaffordable. In NJ, the state exploits the small group market by taking premiums and funding individuals not covered by group insurance.
The best program depends on the business's unique needs and its employees. All groups should offer health insurance as employees are also crushed by inflation. Employees need expert advice to take advantage of any offer and will be more productive, resulting in lower absenteeism from financial loss.
The Inflation Reduction Act is welcome news for individual health participants.
Wednesday, August 24, 2022 Craig E. Chapin
 The Inflation Reduction act guarantees funding to ACA individual insurance market for the next three years with the enhancements implemented by the American Rescue Law of 2021. Premium subsidies are increased for a household earning less than 400% of the Federal Poverty Level (FPL). The "Income Cliff" has been eliminated, limiting costs to homes at any income to 8.5% if not offered group insurance, based on the second lowest silver level plan in their zip code. The "Family Glitch" is removed, limiting a family's cost to 9.12% of household income even when offered group health insurance through work.
Many small employers will embrace the change allowing low-income employees to take advantage of subsidies while continuing to fund health premiums for higher-paid employees that do not qualify for subsidies. An ICHRA will enable employers to set up a special enrollment event to transition employees from group to individual plans.
A families premium cost as a percentage of the federal poverty level
The Inflation Reduction act guarantees funding to ACA individual insurance market for the next three years with the enhancements implemented by the American Rescue Law of 2021. Premium subsidies are increased for a household earning less than 400% of the Federal Poverty Level (FPL). The "Income Cliff" has been eliminated, limiting costs to homes at any income to 8.5% if not offered group insurance, based on the second lowest silver level plan in their zip code. The "Family Glitch" is removed, limiting a family's cost to 9.12% of household income even when offered group health insurance through work.
Many small employers will embrace the change allowing low-income employees to take advantage of subsidies while continuing to fund health premiums for higher-paid employees that do not qualify for subsidies. An ICHRA will enable employers to set up a special enrollment event to transition employees from group to individual plans.
A families premium cost as a percentage of the federal poverty level
 The Inflation Reduction act guarantees funding to ACA individual insurance market for the next three years with the enhancements implemented by the American Rescue Law of 2021. Premium subsidies are increased for a household earning less than 400% of the Federal Poverty Level (FPL). The "Income Cliff" has been eliminated, limiting costs to homes at any income to 8.5% if not offered group insurance, based on the second lowest silver level plan in their zip code. The "Family Glitch" is removed, limiting a family's cost to 9.12% of household income even when offered group health insurance through work.
Many small employers will embrace the change allowing low-income employees to take advantage of subsidies while continuing to fund health premiums for higher-paid employees that do not qualify for subsidies. An ICHRA will enable employers to set up a special enrollment event to transition employees from group to individual plans.
A families premium cost as a percentage of the federal poverty level
The Inflation Reduction act guarantees funding to ACA individual insurance market for the next three years with the enhancements implemented by the American Rescue Law of 2021. Premium subsidies are increased for a household earning less than 400% of the Federal Poverty Level (FPL). The "Income Cliff" has been eliminated, limiting costs to homes at any income to 8.5% if not offered group insurance, based on the second lowest silver level plan in their zip code. The "Family Glitch" is removed, limiting a family's cost to 9.12% of household income even when offered group health insurance through work.
Many small employers will embrace the change allowing low-income employees to take advantage of subsidies while continuing to fund health premiums for higher-paid employees that do not qualify for subsidies. An ICHRA will enable employers to set up a special enrollment event to transition employees from group to individual plans.
A families premium cost as a percentage of the federal poverty level
- 100% to 133%: Zero Premium Plus Cost Sharing Reductions (CSR)
- 133% to 159%: Zero Premium Plus CSR
- 150% to 200%: Zero to 2% Plus CRS
- 200% to 250%: 2% to 4% Plus CRS
- 250% to 300%: 4% to 6%
- 300% to 300%: 6% to 8.5%
- Over 400%: 8.5%
Offering an ICHRA allows families to elect subsidized Health Plans
Tuesday, October 03, 2021
 ICHRA is an employer-funded health benefit that is used to reimburse employees for individual health insurance premiums and healthcare expenses. This exciting benefit gives employers a practical option that creates flexibility and maintains employee satisfaction.
Why is ICHRA such a big deal?
Employers can reimburse employees that do not qualify for Federal subsidies given by the Affordable Care Act and enhanced by the American Rescue Law. With proper plan design, most employees will elect the subsidies for their entire family, so the employer contributes nothing. There are no participation requirements or minimum employer contributions that are part of any group plans. Lastly, the ICHRA allows for a special enrollment event so employers can start a plan any time of the year.
Employee Classes Defined
The ICHRA comes with 11 different employee classes businesses can leverage while structuring benefit eligibility and allowance amounts. The classes separate employees into groups by job-based criteria that include locations, tenure, hours worked, and more. The 11 classes are as follows:
ICHRA is an employer-funded health benefit that is used to reimburse employees for individual health insurance premiums and healthcare expenses. This exciting benefit gives employers a practical option that creates flexibility and maintains employee satisfaction.
Why is ICHRA such a big deal?
Employers can reimburse employees that do not qualify for Federal subsidies given by the Affordable Care Act and enhanced by the American Rescue Law. With proper plan design, most employees will elect the subsidies for their entire family, so the employer contributes nothing. There are no participation requirements or minimum employer contributions that are part of any group plans. Lastly, the ICHRA allows for a special enrollment event so employers can start a plan any time of the year.
Employee Classes Defined
The ICHRA comes with 11 different employee classes businesses can leverage while structuring benefit eligibility and allowance amounts. The classes separate employees into groups by job-based criteria that include locations, tenure, hours worked, and more. The 11 classes are as follows:
- Full-time employees
- Part-time employees
- Salaried employees
- Hourly employees
- Temporary employees of staffing firms
- Seasonal employees
- Employees covered under a collective bargaining agreement
- Employees in a waiting period
- Foreign employees who work abroad
- Employees in different locations, based on rating areas
- A combination of two or more of the above
- 10 employees for employers with fewer than 100 employees
- 10 percent of the total number of employees for employers with between 100 and 200 employees
- 20 employees for employers with more than 200 employees
The ICHRA law gives groups more flexibility.
Friday, October 1, 2021 Craig Chapin
 The ICHRA law allows a large employer to meet ACA mandated premiums contributions while not excluding an employee's dependents from taking advantage of individual subsides. The law gives small groups a special enrollment event to offer more choice to employees and voluntary options for individual health subsidies.
In March 2021, The American Rescue law increased federal subsidies to lower the premiums for individuals not offered group health insurance at work. The law also eliminated the income cliff that restricted premium subsidies for anyone earning over 400% of the Federal Poverty Level. Now any qualified individual will not pay more than 8.5% of their household income for their entire family, and most will pay much less. Many groups want to offer employees savings but are not aware of the rules.
The ICHRA law starts a special enrollment event to enroll employees into individual plans at any time of the year. The law allows employers to contribute to their employee's costs and also contribute to their out-of-pocket costs. Employers can offer employees more choice of plans, better network access, and their dependents have full access to health plans with federal and state subsidies to lower their costs. Employers can use classes to segment their employees with different benefits to accommodate management, out-of-state employees, hourly, seasonal, etc., offering employees lower prices and better network access.
Every group needs to take the time to learn the benefits and rules, and individuals pay on average $10 a month using individual plans verse group premiums of $300 or more.
The ICHRA law allows a large employer to meet ACA mandated premiums contributions while not excluding an employee's dependents from taking advantage of individual subsides. The law gives small groups a special enrollment event to offer more choice to employees and voluntary options for individual health subsidies.
In March 2021, The American Rescue law increased federal subsidies to lower the premiums for individuals not offered group health insurance at work. The law also eliminated the income cliff that restricted premium subsidies for anyone earning over 400% of the Federal Poverty Level. Now any qualified individual will not pay more than 8.5% of their household income for their entire family, and most will pay much less. Many groups want to offer employees savings but are not aware of the rules.
The ICHRA law starts a special enrollment event to enroll employees into individual plans at any time of the year. The law allows employers to contribute to their employee's costs and also contribute to their out-of-pocket costs. Employers can offer employees more choice of plans, better network access, and their dependents have full access to health plans with federal and state subsidies to lower their costs. Employers can use classes to segment their employees with different benefits to accommodate management, out-of-state employees, hourly, seasonal, etc., offering employees lower prices and better network access.
Every group needs to take the time to learn the benefits and rules, and individuals pay on average $10 a month using individual plans verse group premiums of $300 or more.
 The ICHRA law allows a large employer to meet ACA mandated premiums contributions while not excluding an employee's dependents from taking advantage of individual subsides. The law gives small groups a special enrollment event to offer more choice to employees and voluntary options for individual health subsidies.
In March 2021, The American Rescue law increased federal subsidies to lower the premiums for individuals not offered group health insurance at work. The law also eliminated the income cliff that restricted premium subsidies for anyone earning over 400% of the Federal Poverty Level. Now any qualified individual will not pay more than 8.5% of their household income for their entire family, and most will pay much less. Many groups want to offer employees savings but are not aware of the rules.
The ICHRA law starts a special enrollment event to enroll employees into individual plans at any time of the year. The law allows employers to contribute to their employee's costs and also contribute to their out-of-pocket costs. Employers can offer employees more choice of plans, better network access, and their dependents have full access to health plans with federal and state subsidies to lower their costs. Employers can use classes to segment their employees with different benefits to accommodate management, out-of-state employees, hourly, seasonal, etc., offering employees lower prices and better network access.
Every group needs to take the time to learn the benefits and rules, and individuals pay on average $10 a month using individual plans verse group premiums of $300 or more.
The ICHRA law allows a large employer to meet ACA mandated premiums contributions while not excluding an employee's dependents from taking advantage of individual subsides. The law gives small groups a special enrollment event to offer more choice to employees and voluntary options for individual health subsidies.
In March 2021, The American Rescue law increased federal subsidies to lower the premiums for individuals not offered group health insurance at work. The law also eliminated the income cliff that restricted premium subsidies for anyone earning over 400% of the Federal Poverty Level. Now any qualified individual will not pay more than 8.5% of their household income for their entire family, and most will pay much less. Many groups want to offer employees savings but are not aware of the rules.
The ICHRA law starts a special enrollment event to enroll employees into individual plans at any time of the year. The law allows employers to contribute to their employee's costs and also contribute to their out-of-pocket costs. Employers can offer employees more choice of plans, better network access, and their dependents have full access to health plans with federal and state subsidies to lower their costs. Employers can use classes to segment their employees with different benefits to accommodate management, out-of-state employees, hourly, seasonal, etc., offering employees lower prices and better network access.
Every group needs to take the time to learn the benefits and rules, and individuals pay on average $10 a month using individual plans verse group premiums of $300 or more.
Would you prefer to pay $50 or $500 a month?
Tuesday, May 18, 2021 Craig Chapin
 New Jersey residents "Not" offered group health insurance through work save even more with state subsidies in addition to improved Federal subsidies. Many bronze-level individual plans have zero premiums. Family premiums can be less than single plans. Families are also given more choice, with each family member able to pick a different network or plan design. The Affordable Care Act income cliff has been removed, and all eligible households never pay more than 8.5% of their household income, and most pay far less. Everyone in NJ needs to learn their cost at https://enroll.getcovered.nj.gov/hix/preeligibility#/ and notify their employer.
Similar to the Advance Premium Tax Credit (APTC), New Jersey residents will qualify for new savings based on income. Households with annual incomes up to 600% of the FPL will receive the new and expanded NJHPS. An individual with an income of up to $76,560 and a family of four who makes up to $157,200 can receive state subsidies to lower health coverage costs. Anyone who qualifies will be able to see a lower premium when using our plan comparison tool or after filling out an application.
If your employer offers you group health, ask them to learn the detail as they would better serve your interests to cancel the group health and compensate you with better benefits and services.
According to the Kaiser Foundation, Independent study in 2019, employers pay 82% of an average $7,188 single premium and 70% of a $20,576 family premium. With these new subsidies, an entire family's health insurance can be less than the 18% an employer asks employees to pay. Most single employees would rather pay $51 a month versus $100 at work, especially if their employer used the employer's premium savings to give more benefits.
Small employers should establish a competitive edge against the competition, utilizing open enrollment during the summer to educate employees on the change and implement new benefits and services. Don't waste thousands in savings waiting for your group renewal or look to change when so many others renew year-end. Your employees are learning the truth as GetCoveredNJ bombards residents on the news. Be the first to take off your mask with the law in place and the government's permission to proceed.
Employers can take the average $6,000 in employer-paid premium savings and give every employee a defined contribution to purchase benefits and services they want. Don't follow the pack and wait for others to take the lead. Tell your employer to act now as waiting for everyone to take off their mask and following the pack can cost you thousands.
New Jersey residents "Not" offered group health insurance through work save even more with state subsidies in addition to improved Federal subsidies. Many bronze-level individual plans have zero premiums. Family premiums can be less than single plans. Families are also given more choice, with each family member able to pick a different network or plan design. The Affordable Care Act income cliff has been removed, and all eligible households never pay more than 8.5% of their household income, and most pay far less. Everyone in NJ needs to learn their cost at https://enroll.getcovered.nj.gov/hix/preeligibility#/ and notify their employer.
Similar to the Advance Premium Tax Credit (APTC), New Jersey residents will qualify for new savings based on income. Households with annual incomes up to 600% of the FPL will receive the new and expanded NJHPS. An individual with an income of up to $76,560 and a family of four who makes up to $157,200 can receive state subsidies to lower health coverage costs. Anyone who qualifies will be able to see a lower premium when using our plan comparison tool or after filling out an application.
If your employer offers you group health, ask them to learn the detail as they would better serve your interests to cancel the group health and compensate you with better benefits and services.
According to the Kaiser Foundation, Independent study in 2019, employers pay 82% of an average $7,188 single premium and 70% of a $20,576 family premium. With these new subsidies, an entire family's health insurance can be less than the 18% an employer asks employees to pay. Most single employees would rather pay $51 a month versus $100 at work, especially if their employer used the employer's premium savings to give more benefits.
Small employers should establish a competitive edge against the competition, utilizing open enrollment during the summer to educate employees on the change and implement new benefits and services. Don't waste thousands in savings waiting for your group renewal or look to change when so many others renew year-end. Your employees are learning the truth as GetCoveredNJ bombards residents on the news. Be the first to take off your mask with the law in place and the government's permission to proceed.
Employers can take the average $6,000 in employer-paid premium savings and give every employee a defined contribution to purchase benefits and services they want. Don't follow the pack and wait for others to take the lead. Tell your employer to act now as waiting for everyone to take off their mask and following the pack can cost you thousands.
 New Jersey residents "Not" offered group health insurance through work save even more with state subsidies in addition to improved Federal subsidies. Many bronze-level individual plans have zero premiums. Family premiums can be less than single plans. Families are also given more choice, with each family member able to pick a different network or plan design. The Affordable Care Act income cliff has been removed, and all eligible households never pay more than 8.5% of their household income, and most pay far less. Everyone in NJ needs to learn their cost at https://enroll.getcovered.nj.gov/hix/preeligibility#/ and notify their employer.
Similar to the Advance Premium Tax Credit (APTC), New Jersey residents will qualify for new savings based on income. Households with annual incomes up to 600% of the FPL will receive the new and expanded NJHPS. An individual with an income of up to $76,560 and a family of four who makes up to $157,200 can receive state subsidies to lower health coverage costs. Anyone who qualifies will be able to see a lower premium when using our plan comparison tool or after filling out an application.
If your employer offers you group health, ask them to learn the detail as they would better serve your interests to cancel the group health and compensate you with better benefits and services.
According to the Kaiser Foundation, Independent study in 2019, employers pay 82% of an average $7,188 single premium and 70% of a $20,576 family premium. With these new subsidies, an entire family's health insurance can be less than the 18% an employer asks employees to pay. Most single employees would rather pay $51 a month versus $100 at work, especially if their employer used the employer's premium savings to give more benefits.
Small employers should establish a competitive edge against the competition, utilizing open enrollment during the summer to educate employees on the change and implement new benefits and services. Don't waste thousands in savings waiting for your group renewal or look to change when so many others renew year-end. Your employees are learning the truth as GetCoveredNJ bombards residents on the news. Be the first to take off your mask with the law in place and the government's permission to proceed.
Employers can take the average $6,000 in employer-paid premium savings and give every employee a defined contribution to purchase benefits and services they want. Don't follow the pack and wait for others to take the lead. Tell your employer to act now as waiting for everyone to take off their mask and following the pack can cost you thousands.
New Jersey residents "Not" offered group health insurance through work save even more with state subsidies in addition to improved Federal subsidies. Many bronze-level individual plans have zero premiums. Family premiums can be less than single plans. Families are also given more choice, with each family member able to pick a different network or plan design. The Affordable Care Act income cliff has been removed, and all eligible households never pay more than 8.5% of their household income, and most pay far less. Everyone in NJ needs to learn their cost at https://enroll.getcovered.nj.gov/hix/preeligibility#/ and notify their employer.
Similar to the Advance Premium Tax Credit (APTC), New Jersey residents will qualify for new savings based on income. Households with annual incomes up to 600% of the FPL will receive the new and expanded NJHPS. An individual with an income of up to $76,560 and a family of four who makes up to $157,200 can receive state subsidies to lower health coverage costs. Anyone who qualifies will be able to see a lower premium when using our plan comparison tool or after filling out an application.
If your employer offers you group health, ask them to learn the detail as they would better serve your interests to cancel the group health and compensate you with better benefits and services.
According to the Kaiser Foundation, Independent study in 2019, employers pay 82% of an average $7,188 single premium and 70% of a $20,576 family premium. With these new subsidies, an entire family's health insurance can be less than the 18% an employer asks employees to pay. Most single employees would rather pay $51 a month versus $100 at work, especially if their employer used the employer's premium savings to give more benefits.
Small employers should establish a competitive edge against the competition, utilizing open enrollment during the summer to educate employees on the change and implement new benefits and services. Don't waste thousands in savings waiting for your group renewal or look to change when so many others renew year-end. Your employees are learning the truth as GetCoveredNJ bombards residents on the news. Be the first to take off your mask with the law in place and the government's permission to proceed.
Employers can take the average $6,000 in employer-paid premium savings and give every employee a defined contribution to purchase benefits and services they want. Don't follow the pack and wait for others to take the lead. Tell your employer to act now as waiting for everyone to take off their mask and following the pack can cost you thousands.
Give employees more Financial and Wellness protection with Government funding
Thursday, May 1, 2021 Craig E. Chapin
 If you learned, you could pay $500 or $100 for your employee's same health insurance plan. What would you do? Would you give me 15 minutes? Communicating with employers in the post-COVID-19 economy is difficult as remote workers use phone mail and emails as the first line of communication. Employees tell your employers. Owners call now.
Many employers paying for small group health insurance are doing their employees a disservice. However, they are stuck believing there is no better way or don't have the facts. Employee compensation comes in many forms, and with proper education, your employees will cherish the change. While the government pays 75% of any family's health insurance premiums not offered group health insurance, your company paying for group health insurance is obsolete.
Our program is not a trick, but individuals not offered group health insurance get this deal, and we are exploiting it. Don't fight the Fed. Use the premiums savings to compensate employees for other valuable benefits and services. Consider paying your employees differently. They will not disapprove if you give them the money you currently contribute for their group health insurance. Employees will appreciate the change with proper education, especially if you use our system to legally take the money from their pay and automatically pay their insurance premiums each month.
We have a seamless system to transition employees from group health to individual subsidized health insurance. Your company can take credit for giving a defined contribution to employees to pay out-of-pocket medical and dental costs, pay off student loans, child care cost, or save funds in a Health Savings Account.
To utilize these savings, small employers must give up the offer of health insurance, with the compliance obligations on participation, contributions, and continuation. Compensation comes in many forms but raising pay to cover subsided individual plans is not allowed under the Affordable Care Act. However, using a defined contribution for employees to purchase other benefits and services is legal. As a brokerage firm, we can work one-on-one with your employees to enroll families with any carrier in any individual plans. At the same time, our firm can use our traditional group product education and a paperless enrollment system to accumulate employee demographics and educate and enroll employees on any number of benefits and services 24/7 using their smartphones.
A February study shows over 60% of small groups replaced their broker last year for brokers that identified ways to drive down costs and offer better service. Offering non-traditional benefits and increasing productivity by handing over the reins to our technology platform can help your company achieve greater efficiency and allow your company to merge data with payroll and HR administration.
The Post-COVID-19 economy has changed for good. The new administration wants socialized insurance and will pay to get it. Don't try to compete with the Fed but take advantage of the savings. Use our service to simplify the transition while expanding your employee's financial and wellness protection. Productivity will excel, and recruitment and retention will increase.
If you learned, you could pay $500 or $100 for your employee's same health insurance plan. What would you do? Would you give me 15 minutes? Communicating with employers in the post-COVID-19 economy is difficult as remote workers use phone mail and emails as the first line of communication. Employees tell your employers. Owners call now.
Many employers paying for small group health insurance are doing their employees a disservice. However, they are stuck believing there is no better way or don't have the facts. Employee compensation comes in many forms, and with proper education, your employees will cherish the change. While the government pays 75% of any family's health insurance premiums not offered group health insurance, your company paying for group health insurance is obsolete.
Our program is not a trick, but individuals not offered group health insurance get this deal, and we are exploiting it. Don't fight the Fed. Use the premiums savings to compensate employees for other valuable benefits and services. Consider paying your employees differently. They will not disapprove if you give them the money you currently contribute for their group health insurance. Employees will appreciate the change with proper education, especially if you use our system to legally take the money from their pay and automatically pay their insurance premiums each month.
We have a seamless system to transition employees from group health to individual subsidized health insurance. Your company can take credit for giving a defined contribution to employees to pay out-of-pocket medical and dental costs, pay off student loans, child care cost, or save funds in a Health Savings Account.
To utilize these savings, small employers must give up the offer of health insurance, with the compliance obligations on participation, contributions, and continuation. Compensation comes in many forms but raising pay to cover subsided individual plans is not allowed under the Affordable Care Act. However, using a defined contribution for employees to purchase other benefits and services is legal. As a brokerage firm, we can work one-on-one with your employees to enroll families with any carrier in any individual plans. At the same time, our firm can use our traditional group product education and a paperless enrollment system to accumulate employee demographics and educate and enroll employees on any number of benefits and services 24/7 using their smartphones.
A February study shows over 60% of small groups replaced their broker last year for brokers that identified ways to drive down costs and offer better service. Offering non-traditional benefits and increasing productivity by handing over the reins to our technology platform can help your company achieve greater efficiency and allow your company to merge data with payroll and HR administration.
The Post-COVID-19 economy has changed for good. The new administration wants socialized insurance and will pay to get it. Don't try to compete with the Fed but take advantage of the savings. Use our service to simplify the transition while expanding your employee's financial and wellness protection. Productivity will excel, and recruitment and retention will increase.
 If you learned, you could pay $500 or $100 for your employee's same health insurance plan. What would you do? Would you give me 15 minutes? Communicating with employers in the post-COVID-19 economy is difficult as remote workers use phone mail and emails as the first line of communication. Employees tell your employers. Owners call now.
Many employers paying for small group health insurance are doing their employees a disservice. However, they are stuck believing there is no better way or don't have the facts. Employee compensation comes in many forms, and with proper education, your employees will cherish the change. While the government pays 75% of any family's health insurance premiums not offered group health insurance, your company paying for group health insurance is obsolete.
Our program is not a trick, but individuals not offered group health insurance get this deal, and we are exploiting it. Don't fight the Fed. Use the premiums savings to compensate employees for other valuable benefits and services. Consider paying your employees differently. They will not disapprove if you give them the money you currently contribute for their group health insurance. Employees will appreciate the change with proper education, especially if you use our system to legally take the money from their pay and automatically pay their insurance premiums each month.
We have a seamless system to transition employees from group health to individual subsidized health insurance. Your company can take credit for giving a defined contribution to employees to pay out-of-pocket medical and dental costs, pay off student loans, child care cost, or save funds in a Health Savings Account.
To utilize these savings, small employers must give up the offer of health insurance, with the compliance obligations on participation, contributions, and continuation. Compensation comes in many forms but raising pay to cover subsided individual plans is not allowed under the Affordable Care Act. However, using a defined contribution for employees to purchase other benefits and services is legal. As a brokerage firm, we can work one-on-one with your employees to enroll families with any carrier in any individual plans. At the same time, our firm can use our traditional group product education and a paperless enrollment system to accumulate employee demographics and educate and enroll employees on any number of benefits and services 24/7 using their smartphones.
A February study shows over 60% of small groups replaced their broker last year for brokers that identified ways to drive down costs and offer better service. Offering non-traditional benefits and increasing productivity by handing over the reins to our technology platform can help your company achieve greater efficiency and allow your company to merge data with payroll and HR administration.
The Post-COVID-19 economy has changed for good. The new administration wants socialized insurance and will pay to get it. Don't try to compete with the Fed but take advantage of the savings. Use our service to simplify the transition while expanding your employee's financial and wellness protection. Productivity will excel, and recruitment and retention will increase.
If you learned, you could pay $500 or $100 for your employee's same health insurance plan. What would you do? Would you give me 15 minutes? Communicating with employers in the post-COVID-19 economy is difficult as remote workers use phone mail and emails as the first line of communication. Employees tell your employers. Owners call now.
Many employers paying for small group health insurance are doing their employees a disservice. However, they are stuck believing there is no better way or don't have the facts. Employee compensation comes in many forms, and with proper education, your employees will cherish the change. While the government pays 75% of any family's health insurance premiums not offered group health insurance, your company paying for group health insurance is obsolete.
Our program is not a trick, but individuals not offered group health insurance get this deal, and we are exploiting it. Don't fight the Fed. Use the premiums savings to compensate employees for other valuable benefits and services. Consider paying your employees differently. They will not disapprove if you give them the money you currently contribute for their group health insurance. Employees will appreciate the change with proper education, especially if you use our system to legally take the money from their pay and automatically pay their insurance premiums each month.
We have a seamless system to transition employees from group health to individual subsidized health insurance. Your company can take credit for giving a defined contribution to employees to pay out-of-pocket medical and dental costs, pay off student loans, child care cost, or save funds in a Health Savings Account.
To utilize these savings, small employers must give up the offer of health insurance, with the compliance obligations on participation, contributions, and continuation. Compensation comes in many forms but raising pay to cover subsided individual plans is not allowed under the Affordable Care Act. However, using a defined contribution for employees to purchase other benefits and services is legal. As a brokerage firm, we can work one-on-one with your employees to enroll families with any carrier in any individual plans. At the same time, our firm can use our traditional group product education and a paperless enrollment system to accumulate employee demographics and educate and enroll employees on any number of benefits and services 24/7 using their smartphones.
A February study shows over 60% of small groups replaced their broker last year for brokers that identified ways to drive down costs and offer better service. Offering non-traditional benefits and increasing productivity by handing over the reins to our technology platform can help your company achieve greater efficiency and allow your company to merge data with payroll and HR administration.
The Post-COVID-19 economy has changed for good. The new administration wants socialized insurance and will pay to get it. Don't try to compete with the Fed but take advantage of the savings. Use our service to simplify the transition while expanding your employee's financial and wellness protection. Productivity will excel, and recruitment and retention will increase.
The American Rescue Plan Makes Group Health Obsolete
Monday, March 11, 2021 Craig E. Chapin
 The American Rescue Bill was signed into law on March 11, 2021, vastly changing individual health coverage subsidies. The new subsidies are fully funded for two years, but we feel this new entitlement will be continued at least while President Biden is in office. He ran on fixing Obamacare, and this is the first step.
Planned or not, the savings are so significant that employers should consider canceling their group health plans and compensating their employees with the premium saving. An employer can eliminate complying with COBRA, and Family leaves laws. Employees would have a wider choice on plan design, dependents would not be cut out from subsidies, and employers would not have to comply with minimum premium contributions or participation requirements.
The list of enhanced supplements and tax savings vehicles is broad and just another form of compensation. Some employees would benefit from first dollar benefits funding into a flexible spending account or health savings account. Others may want an accident, dental, disability, cancer, critical illness, life, long-term care, and vision insurance. Students may wish to pay off their student loans or want more reimbursements for remote offices, including cell phone and internet costs. All of these benefits can be offered on an employer or employee-paid basis.
We have a system to educate workers and transition them to individual plans. Our program allows an employer to offer an online platform offering a complete package of customized services and supplemental plans.
Studies show that employees desire benefits second to compensation. A more comprehensive choice of services gives small employers the upper hand when recruiting new help and retaining valued workers. Don't try to complete with Federal subsidies and use the savings to provide more first dollar benefits to your employees. Entitlement programs may change but generally never disappear.
The American Rescue Bill was signed into law on March 11, 2021, vastly changing individual health coverage subsidies. The new subsidies are fully funded for two years, but we feel this new entitlement will be continued at least while President Biden is in office. He ran on fixing Obamacare, and this is the first step.
Planned or not, the savings are so significant that employers should consider canceling their group health plans and compensating their employees with the premium saving. An employer can eliminate complying with COBRA, and Family leaves laws. Employees would have a wider choice on plan design, dependents would not be cut out from subsidies, and employers would not have to comply with minimum premium contributions or participation requirements.
The list of enhanced supplements and tax savings vehicles is broad and just another form of compensation. Some employees would benefit from first dollar benefits funding into a flexible spending account or health savings account. Others may want an accident, dental, disability, cancer, critical illness, life, long-term care, and vision insurance. Students may wish to pay off their student loans or want more reimbursements for remote offices, including cell phone and internet costs. All of these benefits can be offered on an employer or employee-paid basis.
We have a system to educate workers and transition them to individual plans. Our program allows an employer to offer an online platform offering a complete package of customized services and supplemental plans.
Studies show that employees desire benefits second to compensation. A more comprehensive choice of services gives small employers the upper hand when recruiting new help and retaining valued workers. Don't try to complete with Federal subsidies and use the savings to provide more first dollar benefits to your employees. Entitlement programs may change but generally never disappear.
 The American Rescue Bill was signed into law on March 11, 2021, vastly changing individual health coverage subsidies. The new subsidies are fully funded for two years, but we feel this new entitlement will be continued at least while President Biden is in office. He ran on fixing Obamacare, and this is the first step.
Planned or not, the savings are so significant that employers should consider canceling their group health plans and compensating their employees with the premium saving. An employer can eliminate complying with COBRA, and Family leaves laws. Employees would have a wider choice on plan design, dependents would not be cut out from subsidies, and employers would not have to comply with minimum premium contributions or participation requirements.
The list of enhanced supplements and tax savings vehicles is broad and just another form of compensation. Some employees would benefit from first dollar benefits funding into a flexible spending account or health savings account. Others may want an accident, dental, disability, cancer, critical illness, life, long-term care, and vision insurance. Students may wish to pay off their student loans or want more reimbursements for remote offices, including cell phone and internet costs. All of these benefits can be offered on an employer or employee-paid basis.
We have a system to educate workers and transition them to individual plans. Our program allows an employer to offer an online platform offering a complete package of customized services and supplemental plans.
Studies show that employees desire benefits second to compensation. A more comprehensive choice of services gives small employers the upper hand when recruiting new help and retaining valued workers. Don't try to complete with Federal subsidies and use the savings to provide more first dollar benefits to your employees. Entitlement programs may change but generally never disappear.
The American Rescue Bill was signed into law on March 11, 2021, vastly changing individual health coverage subsidies. The new subsidies are fully funded for two years, but we feel this new entitlement will be continued at least while President Biden is in office. He ran on fixing Obamacare, and this is the first step.
Planned or not, the savings are so significant that employers should consider canceling their group health plans and compensating their employees with the premium saving. An employer can eliminate complying with COBRA, and Family leaves laws. Employees would have a wider choice on plan design, dependents would not be cut out from subsidies, and employers would not have to comply with minimum premium contributions or participation requirements.
The list of enhanced supplements and tax savings vehicles is broad and just another form of compensation. Some employees would benefit from first dollar benefits funding into a flexible spending account or health savings account. Others may want an accident, dental, disability, cancer, critical illness, life, long-term care, and vision insurance. Students may wish to pay off their student loans or want more reimbursements for remote offices, including cell phone and internet costs. All of these benefits can be offered on an employer or employee-paid basis.
We have a system to educate workers and transition them to individual plans. Our program allows an employer to offer an online platform offering a complete package of customized services and supplemental plans.
Studies show that employees desire benefits second to compensation. A more comprehensive choice of services gives small employers the upper hand when recruiting new help and retaining valued workers. Don't try to complete with Federal subsidies and use the savings to provide more first dollar benefits to your employees. Entitlement programs may change but generally never disappear.
Remote work can be beneficial for employees and companies.
Thursday, October 01, 2020 Craig Chapin
 Many workers enjoy the benefits of telecommuting, and companies are seeing an increase in productivity. Automation technology promises to relieve the stress workers experience from the bigger workloads due to the human labor shortage of higher-skilled jobs. Eventually, the economy will rebound, and you'll need to resume hiring additional staff. 1 Stop Benefits is helping our customers by offering the Ease small group onboarding and enrollment system at no cost.
With more employees working remotely, you need to have a system to send job offers, highlight company benefits, and any employee costs. Your organization may also realize that recruiting might be easier when tapping talent from regions outside your location. With remote work, you may want to track time off, vacations and expenses. Our system collects employee I9, W4, direct deposit forms and allows employees to change their profiles. Educate employees with videos, graphic comparisons while enrolling into eligible benefits after satisfying any waiting periods. Special enrollment changes and address changes are easily implemented, tracked paperlessly. The Ease system can merge employee's data with payroll, stay compliant with ACA reporting, and add HR support throughout the year.
Small businesses need to automate to reduce administration and save money. How important is it for you to eliminate paper, eliminate duplicate entry, and have data stored in one secure system with access 24/7? Would you like to give your workers more financial protection without time-consuming meetings? Let our trained consultants answer all their questions? Allow us to survey your employee's desire for health and financial wellness benefits.
Ask for a demo of our services beyond offering quality health insurance. Does your consultant offer you a complete system to take the administration of benefits off your hands and automate services 24/7? The Ease system is easy to implement, and you can start with a call to 1 Stop Benefits.
Many workers enjoy the benefits of telecommuting, and companies are seeing an increase in productivity. Automation technology promises to relieve the stress workers experience from the bigger workloads due to the human labor shortage of higher-skilled jobs. Eventually, the economy will rebound, and you'll need to resume hiring additional staff. 1 Stop Benefits is helping our customers by offering the Ease small group onboarding and enrollment system at no cost.
With more employees working remotely, you need to have a system to send job offers, highlight company benefits, and any employee costs. Your organization may also realize that recruiting might be easier when tapping talent from regions outside your location. With remote work, you may want to track time off, vacations and expenses. Our system collects employee I9, W4, direct deposit forms and allows employees to change their profiles. Educate employees with videos, graphic comparisons while enrolling into eligible benefits after satisfying any waiting periods. Special enrollment changes and address changes are easily implemented, tracked paperlessly. The Ease system can merge employee's data with payroll, stay compliant with ACA reporting, and add HR support throughout the year.
Small businesses need to automate to reduce administration and save money. How important is it for you to eliminate paper, eliminate duplicate entry, and have data stored in one secure system with access 24/7? Would you like to give your workers more financial protection without time-consuming meetings? Let our trained consultants answer all their questions? Allow us to survey your employee's desire for health and financial wellness benefits.
Ask for a demo of our services beyond offering quality health insurance. Does your consultant offer you a complete system to take the administration of benefits off your hands and automate services 24/7? The Ease system is easy to implement, and you can start with a call to 1 Stop Benefits.
 Many workers enjoy the benefits of telecommuting, and companies are seeing an increase in productivity. Automation technology promises to relieve the stress workers experience from the bigger workloads due to the human labor shortage of higher-skilled jobs. Eventually, the economy will rebound, and you'll need to resume hiring additional staff. 1 Stop Benefits is helping our customers by offering the Ease small group onboarding and enrollment system at no cost.
With more employees working remotely, you need to have a system to send job offers, highlight company benefits, and any employee costs. Your organization may also realize that recruiting might be easier when tapping talent from regions outside your location. With remote work, you may want to track time off, vacations and expenses. Our system collects employee I9, W4, direct deposit forms and allows employees to change their profiles. Educate employees with videos, graphic comparisons while enrolling into eligible benefits after satisfying any waiting periods. Special enrollment changes and address changes are easily implemented, tracked paperlessly. The Ease system can merge employee's data with payroll, stay compliant with ACA reporting, and add HR support throughout the year.
Small businesses need to automate to reduce administration and save money. How important is it for you to eliminate paper, eliminate duplicate entry, and have data stored in one secure system with access 24/7? Would you like to give your workers more financial protection without time-consuming meetings? Let our trained consultants answer all their questions? Allow us to survey your employee's desire for health and financial wellness benefits.
Ask for a demo of our services beyond offering quality health insurance. Does your consultant offer you a complete system to take the administration of benefits off your hands and automate services 24/7? The Ease system is easy to implement, and you can start with a call to 1 Stop Benefits.
Many workers enjoy the benefits of telecommuting, and companies are seeing an increase in productivity. Automation technology promises to relieve the stress workers experience from the bigger workloads due to the human labor shortage of higher-skilled jobs. Eventually, the economy will rebound, and you'll need to resume hiring additional staff. 1 Stop Benefits is helping our customers by offering the Ease small group onboarding and enrollment system at no cost.
With more employees working remotely, you need to have a system to send job offers, highlight company benefits, and any employee costs. Your organization may also realize that recruiting might be easier when tapping talent from regions outside your location. With remote work, you may want to track time off, vacations and expenses. Our system collects employee I9, W4, direct deposit forms and allows employees to change their profiles. Educate employees with videos, graphic comparisons while enrolling into eligible benefits after satisfying any waiting periods. Special enrollment changes and address changes are easily implemented, tracked paperlessly. The Ease system can merge employee's data with payroll, stay compliant with ACA reporting, and add HR support throughout the year.
Small businesses need to automate to reduce administration and save money. How important is it for you to eliminate paper, eliminate duplicate entry, and have data stored in one secure system with access 24/7? Would you like to give your workers more financial protection without time-consuming meetings? Let our trained consultants answer all their questions? Allow us to survey your employee's desire for health and financial wellness benefits.
Ask for a demo of our services beyond offering quality health insurance. Does your consultant offer you a complete system to take the administration of benefits off your hands and automate services 24/7? The Ease system is easy to implement, and you can start with a call to 1 Stop Benefits.
Your Employees are being impacted by Financial Stress
Monday, February 24, 2020 Craig E. Chapin
 In a 2019 MetLife report, one in three employees said that personal financial stress interfered with their job performance - and overall, employees flagged personal finance as the main source of stress in their lives. Every company should consider offering the One Stop Benefits Calculator to lower employee's stress levels.
Employers reported a loss of $250 billion in 2019 due to employee stress. It's estimated that financial stress costs roughly 1,922 hours and $28,830 in lost weekly healthcare productivity in a company of 10,000 - that's 99,944 hours and $1,499,160 a year down the drain. Other studies show employers losing 11% to 14% of their overall annual payroll due to lost productivity and higher absenteeism.
Not having an emergency fund is the top-cited worry for millennials and Gen Xers, while half of all employees across generations live paycheck to paycheck. Employees clearly see that their benefits are an answer to at least some of their problems: 37% of millennials said student loan repayment was the perk they most wanted from employers, while 30% of Gen Xers and 28% of baby boomers mostly wanted financial wellness benefits with access to financial counselors.
Financial wellness is not a one-size-fits-all solution. While it's clear most employees share the desire for financial wellness benefits, there's no single product or service that addresses every individual's unique combination of financial stressors. Rather, the employer's goal should be to thoughtfully provide options, along with support, so participants can choose a frictionless path forward.
A whopping 80% of employees want financial planning workshops or financial wellness tools from their employers, but only 20% of employers offer these programs. Providing education and advice may be a good place to start, but don't forget to take a hard look at products, services, and relationships with outside vendors. While most employees wish their companies offered student loan repayment benefits, yet only 4% of them do.
All size businesses are affected, and this can be the number one reason employees are losing sleep, and that directly impacts your business.
In a 2019 MetLife report, one in three employees said that personal financial stress interfered with their job performance - and overall, employees flagged personal finance as the main source of stress in their lives. Every company should consider offering the One Stop Benefits Calculator to lower employee's stress levels.
Employers reported a loss of $250 billion in 2019 due to employee stress. It's estimated that financial stress costs roughly 1,922 hours and $28,830 in lost weekly healthcare productivity in a company of 10,000 - that's 99,944 hours and $1,499,160 a year down the drain. Other studies show employers losing 11% to 14% of their overall annual payroll due to lost productivity and higher absenteeism.
Not having an emergency fund is the top-cited worry for millennials and Gen Xers, while half of all employees across generations live paycheck to paycheck. Employees clearly see that their benefits are an answer to at least some of their problems: 37% of millennials said student loan repayment was the perk they most wanted from employers, while 30% of Gen Xers and 28% of baby boomers mostly wanted financial wellness benefits with access to financial counselors.
Financial wellness is not a one-size-fits-all solution. While it's clear most employees share the desire for financial wellness benefits, there's no single product or service that addresses every individual's unique combination of financial stressors. Rather, the employer's goal should be to thoughtfully provide options, along with support, so participants can choose a frictionless path forward.
A whopping 80% of employees want financial planning workshops or financial wellness tools from their employers, but only 20% of employers offer these programs. Providing education and advice may be a good place to start, but don't forget to take a hard look at products, services, and relationships with outside vendors. While most employees wish their companies offered student loan repayment benefits, yet only 4% of them do.
All size businesses are affected, and this can be the number one reason employees are losing sleep, and that directly impacts your business.
 In a 2019 MetLife report, one in three employees said that personal financial stress interfered with their job performance - and overall, employees flagged personal finance as the main source of stress in their lives. Every company should consider offering the One Stop Benefits Calculator to lower employee's stress levels.
Employers reported a loss of $250 billion in 2019 due to employee stress. It's estimated that financial stress costs roughly 1,922 hours and $28,830 in lost weekly healthcare productivity in a company of 10,000 - that's 99,944 hours and $1,499,160 a year down the drain. Other studies show employers losing 11% to 14% of their overall annual payroll due to lost productivity and higher absenteeism.
Not having an emergency fund is the top-cited worry for millennials and Gen Xers, while half of all employees across generations live paycheck to paycheck. Employees clearly see that their benefits are an answer to at least some of their problems: 37% of millennials said student loan repayment was the perk they most wanted from employers, while 30% of Gen Xers and 28% of baby boomers mostly wanted financial wellness benefits with access to financial counselors.
Financial wellness is not a one-size-fits-all solution. While it's clear most employees share the desire for financial wellness benefits, there's no single product or service that addresses every individual's unique combination of financial stressors. Rather, the employer's goal should be to thoughtfully provide options, along with support, so participants can choose a frictionless path forward.
A whopping 80% of employees want financial planning workshops or financial wellness tools from their employers, but only 20% of employers offer these programs. Providing education and advice may be a good place to start, but don't forget to take a hard look at products, services, and relationships with outside vendors. While most employees wish their companies offered student loan repayment benefits, yet only 4% of them do.
All size businesses are affected, and this can be the number one reason employees are losing sleep, and that directly impacts your business.
In a 2019 MetLife report, one in three employees said that personal financial stress interfered with their job performance - and overall, employees flagged personal finance as the main source of stress in their lives. Every company should consider offering the One Stop Benefits Calculator to lower employee's stress levels.
Employers reported a loss of $250 billion in 2019 due to employee stress. It's estimated that financial stress costs roughly 1,922 hours and $28,830 in lost weekly healthcare productivity in a company of 10,000 - that's 99,944 hours and $1,499,160 a year down the drain. Other studies show employers losing 11% to 14% of their overall annual payroll due to lost productivity and higher absenteeism.
Not having an emergency fund is the top-cited worry for millennials and Gen Xers, while half of all employees across generations live paycheck to paycheck. Employees clearly see that their benefits are an answer to at least some of their problems: 37% of millennials said student loan repayment was the perk they most wanted from employers, while 30% of Gen Xers and 28% of baby boomers mostly wanted financial wellness benefits with access to financial counselors.
Financial wellness is not a one-size-fits-all solution. While it's clear most employees share the desire for financial wellness benefits, there's no single product or service that addresses every individual's unique combination of financial stressors. Rather, the employer's goal should be to thoughtfully provide options, along with support, so participants can choose a frictionless path forward.
A whopping 80% of employees want financial planning workshops or financial wellness tools from their employers, but only 20% of employers offer these programs. Providing education and advice may be a good place to start, but don't forget to take a hard look at products, services, and relationships with outside vendors. While most employees wish their companies offered student loan repayment benefits, yet only 4% of them do.
All size businesses are affected, and this can be the number one reason employees are losing sleep, and that directly impacts your business.
Reasons to use permanent Life Insurance for Retirement planning.
Monday, January 13, 2020 Ed Scott and Craig Chapin
 Life insurance is a good asset versus an IRA according to Ed Scott a tax advisor, published in Feb 2016. Based on my three decades of experience I feel his statements still hold true. In addition, the expansion of the living benefits of chronic, critical and long-term care on new life insurance contracts offers additional protection to advance up to 90% of the face value of coverage using term or permanent life insurance as a result of an illness or accident that shortened your life expectancy.
Ed Scott stated I do not sell life insurance. I am a tax advisor. And as a tax advisor, I can tell you that the single biggest benefit in the federal tax code is the income tax exemption for life insurance. Life Insurance should be a bedrock of any serious financial, retirement or estate plan, but it is not used nearly enough, even by those advisors who do sell life insurance. For planning purposes here, I refer only to permanent insurance, not term insurance.
Obviously, life insurance provides an income tax-free death benefit and people understand that. But besides the death benefit, here are your five best points for encouraging more people to have life insurance to enhance their long-term financial security.
1. IRAs are bad assets; life insurance is a good asset
Most people have their retirement savings in IRAs and 401(k)s. These are bad assets because they are tax-deferred. The tax will one day have to be paid, creating a growing debt on these retirement savings. The future tax will be paid when the money is needed most, in retirement, and at an unknown, but probably higher tax rate.
This makes these traditional retirement accounts an uncertain and diminishing asset over time. Replacing these accounts over time with permanent life insurance turns these tax-deferred funds into tax-free savings. Clients should begin a program of systematic IRA withdrawals to decrease their IRA balances and plow those funds into permanent life insurance.
This tax will have to be paid anyway beginning at age 70 1/2 and probably at a higher rate on a higher balance. So it's best to deal with this now to have more retirement funds available long-term. The increasing and uncertain tax debt is paid off by paying the tax now at known tax rates, which are at historic lows right now, while income tax-free savings are growing in the permanent insurance policy.
2. Life Insurance is an investment, not an expense
People will say life insurance costs too much. Moving funds either from IRAs or from other accounts to permanent life insurance is not an expense; it's an investment in a better long-term asset. Yes, if the funds are withdrawn from an IRA, there will be a tax to pay, but that tax will have had to be paid at some point anyway, probably at higher tax rates in the future.
Once the funds are in a permanent life insurance policy, they are simply located in a different and far better long-term asset than an IRA or 401(k). The funds in that new location, the life insurance policy, remove not only the tax risk but can also eliminate the stock market risk, depending on how the policy is set up.
That's a big deal in retirement, and something you generally cannot do in a traditional IRA. If you were changing investments, you would not think of that as an expense, so the same applies here.
3. Life insurance has lifetime benefits
People think of life insurance for the death benefit, but most people don't know about the powerful lifetime retirement and tax benefits. Funds in a permanent life insurance policy can double as a retirement savings account, but without the worry about what future tax rates will be.
If these funds are needed in retirement, they are accessible, tax- and penalty-free. That is a big deal because if the funds were in an IRA, distributions would not only be taxable (in a traditional IRA), but that increased income could trigger other so-called "stealth taxes."
These are hidden tax increases in the form of phased-out deductions, tax credits, exemptions, and other benefits as income increases. For example, an income increase from an IRA distribution could cause more Social Security benefits to be taxable or trigger the 3.8 percent additional tax on net investment income from capital gains, interest, and dividends.
Accessing funds from a life insurance policy are tax-free (up to cost-basis, and after that if taken as policy loans against the tax-free death benefit) so they don't increase income. And in fact, the withdrawals keep taxable income and taxes lower in retirement. These are valuable lifetime benefits, in addition to the death benefit.
4. More Control with Life Insurance
IRAs are subject to annual required minimum distributions (RMDs) after age 70 1/2, whether the money is needed or not (Roth IRAs are exempt from lifetime RMDs). This causes forced distributions and additional taxes, though the client may not need or want to withdraw those funds.
These forced withdrawals take control away, while withdrawing from the value in a life insurance policy can be done at any time, or not. Clients are in control of their retirement savings in a life insurance policy.
5. Powerful wealth creation through leverage
Life insurance creates more long-term wealth than any other investment. And because this wealth is income tax-free, it is much more valuable than tax-deferred retirement savings that are at the mercy of future higher tax rates.
It's the leverage that creates wealth. Life insurance is the only investment where one dollar can do the work of many, and the result is guaranteed and tax-free. With an IRA, for example, it would take many years to multiply that balance; and when it is withdrawn, it will be diminished by taxes.
Taking the same funds that were in an IRA and investing them (after-the tax was paid on the IRA distribution) in a permanent life insurance policy, would produce many multiples of that original IRA balance, and it would be tax-free, not only for use during life but especially if there were an early death.
Finding the money to pay for life insurance
1 Stop Benefits is uniquely able to secure life insurance coverage at just about any age. We have individual plans that guaranteed coverage up to $100,000 if you are actively at work or smaller amounts id not able to work regardless of health, weight, or occupation. Of course, it is to your advantage to purchase early or without a pre-existing condition.
Leveraging your bad assets to pay for good assets should be your New Year's resolution. If you have money tied up in none performing stocks, under leverage property, are over 59 1/2, you have sources to pay premiums. Consider the need for cash in the future for long-term care especially if you do not have separate coverage or want to live out your life in your home.
Life insurance is a good asset versus an IRA according to Ed Scott a tax advisor, published in Feb 2016. Based on my three decades of experience I feel his statements still hold true. In addition, the expansion of the living benefits of chronic, critical and long-term care on new life insurance contracts offers additional protection to advance up to 90% of the face value of coverage using term or permanent life insurance as a result of an illness or accident that shortened your life expectancy.
Ed Scott stated I do not sell life insurance. I am a tax advisor. And as a tax advisor, I can tell you that the single biggest benefit in the federal tax code is the income tax exemption for life insurance. Life Insurance should be a bedrock of any serious financial, retirement or estate plan, but it is not used nearly enough, even by those advisors who do sell life insurance. For planning purposes here, I refer only to permanent insurance, not term insurance.
Obviously, life insurance provides an income tax-free death benefit and people understand that. But besides the death benefit, here are your five best points for encouraging more people to have life insurance to enhance their long-term financial security.
1. IRAs are bad assets; life insurance is a good asset
Most people have their retirement savings in IRAs and 401(k)s. These are bad assets because they are tax-deferred. The tax will one day have to be paid, creating a growing debt on these retirement savings. The future tax will be paid when the money is needed most, in retirement, and at an unknown, but probably higher tax rate.
This makes these traditional retirement accounts an uncertain and diminishing asset over time. Replacing these accounts over time with permanent life insurance turns these tax-deferred funds into tax-free savings. Clients should begin a program of systematic IRA withdrawals to decrease their IRA balances and plow those funds into permanent life insurance.
This tax will have to be paid anyway beginning at age 70 1/2 and probably at a higher rate on a higher balance. So it's best to deal with this now to have more retirement funds available long-term. The increasing and uncertain tax debt is paid off by paying the tax now at known tax rates, which are at historic lows right now, while income tax-free savings are growing in the permanent insurance policy.
2. Life Insurance is an investment, not an expense
People will say life insurance costs too much. Moving funds either from IRAs or from other accounts to permanent life insurance is not an expense; it's an investment in a better long-term asset. Yes, if the funds are withdrawn from an IRA, there will be a tax to pay, but that tax will have had to be paid at some point anyway, probably at higher tax rates in the future.
Once the funds are in a permanent life insurance policy, they are simply located in a different and far better long-term asset than an IRA or 401(k). The funds in that new location, the life insurance policy, remove not only the tax risk but can also eliminate the stock market risk, depending on how the policy is set up.
That's a big deal in retirement, and something you generally cannot do in a traditional IRA. If you were changing investments, you would not think of that as an expense, so the same applies here.
3. Life insurance has lifetime benefits
People think of life insurance for the death benefit, but most people don't know about the powerful lifetime retirement and tax benefits. Funds in a permanent life insurance policy can double as a retirement savings account, but without the worry about what future tax rates will be.
If these funds are needed in retirement, they are accessible, tax- and penalty-free. That is a big deal because if the funds were in an IRA, distributions would not only be taxable (in a traditional IRA), but that increased income could trigger other so-called "stealth taxes."
These are hidden tax increases in the form of phased-out deductions, tax credits, exemptions, and other benefits as income increases. For example, an income increase from an IRA distribution could cause more Social Security benefits to be taxable or trigger the 3.8 percent additional tax on net investment income from capital gains, interest, and dividends.
Accessing funds from a life insurance policy are tax-free (up to cost-basis, and after that if taken as policy loans against the tax-free death benefit) so they don't increase income. And in fact, the withdrawals keep taxable income and taxes lower in retirement. These are valuable lifetime benefits, in addition to the death benefit.
4. More Control with Life Insurance
IRAs are subject to annual required minimum distributions (RMDs) after age 70 1/2, whether the money is needed or not (Roth IRAs are exempt from lifetime RMDs). This causes forced distributions and additional taxes, though the client may not need or want to withdraw those funds.
These forced withdrawals take control away, while withdrawing from the value in a life insurance policy can be done at any time, or not. Clients are in control of their retirement savings in a life insurance policy.
5. Powerful wealth creation through leverage
Life insurance creates more long-term wealth than any other investment. And because this wealth is income tax-free, it is much more valuable than tax-deferred retirement savings that are at the mercy of future higher tax rates.
It's the leverage that creates wealth. Life insurance is the only investment where one dollar can do the work of many, and the result is guaranteed and tax-free. With an IRA, for example, it would take many years to multiply that balance; and when it is withdrawn, it will be diminished by taxes.
Taking the same funds that were in an IRA and investing them (after-the tax was paid on the IRA distribution) in a permanent life insurance policy, would produce many multiples of that original IRA balance, and it would be tax-free, not only for use during life but especially if there were an early death.
Finding the money to pay for life insurance
1 Stop Benefits is uniquely able to secure life insurance coverage at just about any age. We have individual plans that guaranteed coverage up to $100,000 if you are actively at work or smaller amounts id not able to work regardless of health, weight, or occupation. Of course, it is to your advantage to purchase early or without a pre-existing condition.
Leveraging your bad assets to pay for good assets should be your New Year's resolution. If you have money tied up in none performing stocks, under leverage property, are over 59 1/2, you have sources to pay premiums. Consider the need for cash in the future for long-term care especially if you do not have separate coverage or want to live out your life in your home.
 Life insurance is a good asset versus an IRA according to Ed Scott a tax advisor, published in Feb 2016. Based on my three decades of experience I feel his statements still hold true. In addition, the expansion of the living benefits of chronic, critical and long-term care on new life insurance contracts offers additional protection to advance up to 90% of the face value of coverage using term or permanent life insurance as a result of an illness or accident that shortened your life expectancy.
Ed Scott stated I do not sell life insurance. I am a tax advisor. And as a tax advisor, I can tell you that the single biggest benefit in the federal tax code is the income tax exemption for life insurance. Life Insurance should be a bedrock of any serious financial, retirement or estate plan, but it is not used nearly enough, even by those advisors who do sell life insurance. For planning purposes here, I refer only to permanent insurance, not term insurance.
Obviously, life insurance provides an income tax-free death benefit and people understand that. But besides the death benefit, here are your five best points for encouraging more people to have life insurance to enhance their long-term financial security.
1. IRAs are bad assets; life insurance is a good asset
Most people have their retirement savings in IRAs and 401(k)s. These are bad assets because they are tax-deferred. The tax will one day have to be paid, creating a growing debt on these retirement savings. The future tax will be paid when the money is needed most, in retirement, and at an unknown, but probably higher tax rate.
This makes these traditional retirement accounts an uncertain and diminishing asset over time. Replacing these accounts over time with permanent life insurance turns these tax-deferred funds into tax-free savings. Clients should begin a program of systematic IRA withdrawals to decrease their IRA balances and plow those funds into permanent life insurance.
This tax will have to be paid anyway beginning at age 70 1/2 and probably at a higher rate on a higher balance. So it's best to deal with this now to have more retirement funds available long-term. The increasing and uncertain tax debt is paid off by paying the tax now at known tax rates, which are at historic lows right now, while income tax-free savings are growing in the permanent insurance policy.
2. Life Insurance is an investment, not an expense
People will say life insurance costs too much. Moving funds either from IRAs or from other accounts to permanent life insurance is not an expense; it's an investment in a better long-term asset. Yes, if the funds are withdrawn from an IRA, there will be a tax to pay, but that tax will have had to be paid at some point anyway, probably at higher tax rates in the future.
Once the funds are in a permanent life insurance policy, they are simply located in a different and far better long-term asset than an IRA or 401(k). The funds in that new location, the life insurance policy, remove not only the tax risk but can also eliminate the stock market risk, depending on how the policy is set up.
That's a big deal in retirement, and something you generally cannot do in a traditional IRA. If you were changing investments, you would not think of that as an expense, so the same applies here.
3. Life insurance has lifetime benefits
People think of life insurance for the death benefit, but most people don't know about the powerful lifetime retirement and tax benefits. Funds in a permanent life insurance policy can double as a retirement savings account, but without the worry about what future tax rates will be.
If these funds are needed in retirement, they are accessible, tax- and penalty-free. That is a big deal because if the funds were in an IRA, distributions would not only be taxable (in a traditional IRA), but that increased income could trigger other so-called "stealth taxes."
These are hidden tax increases in the form of phased-out deductions, tax credits, exemptions, and other benefits as income increases. For example, an income increase from an IRA distribution could cause more Social Security benefits to be taxable or trigger the 3.8 percent additional tax on net investment income from capital gains, interest, and dividends.
Accessing funds from a life insurance policy are tax-free (up to cost-basis, and after that if taken as policy loans against the tax-free death benefit) so they don't increase income. And in fact, the withdrawals keep taxable income and taxes lower in retirement. These are valuable lifetime benefits, in addition to the death benefit.
4. More Control with Life Insurance
IRAs are subject to annual required minimum distributions (RMDs) after age 70 1/2, whether the money is needed or not (Roth IRAs are exempt from lifetime RMDs). This causes forced distributions and additional taxes, though the client may not need or want to withdraw those funds.
These forced withdrawals take control away, while withdrawing from the value in a life insurance policy can be done at any time, or not. Clients are in control of their retirement savings in a life insurance policy.
5. Powerful wealth creation through leverage
Life insurance creates more long-term wealth than any other investment. And because this wealth is income tax-free, it is much more valuable than tax-deferred retirement savings that are at the mercy of future higher tax rates.
It's the leverage that creates wealth. Life insurance is the only investment where one dollar can do the work of many, and the result is guaranteed and tax-free. With an IRA, for example, it would take many years to multiply that balance; and when it is withdrawn, it will be diminished by taxes.
Taking the same funds that were in an IRA and investing them (after-the tax was paid on the IRA distribution) in a permanent life insurance policy, would produce many multiples of that original IRA balance, and it would be tax-free, not only for use during life but especially if there were an early death.
Finding the money to pay for life insurance
1 Stop Benefits is uniquely able to secure life insurance coverage at just about any age. We have individual plans that guaranteed coverage up to $100,000 if you are actively at work or smaller amounts id not able to work regardless of health, weight, or occupation. Of course, it is to your advantage to purchase early or without a pre-existing condition.
Leveraging your bad assets to pay for good assets should be your New Year's resolution. If you have money tied up in none performing stocks, under leverage property, are over 59 1/2, you have sources to pay premiums. Consider the need for cash in the future for long-term care especially if you do not have separate coverage or want to live out your life in your home.
Life insurance is a good asset versus an IRA according to Ed Scott a tax advisor, published in Feb 2016. Based on my three decades of experience I feel his statements still hold true. In addition, the expansion of the living benefits of chronic, critical and long-term care on new life insurance contracts offers additional protection to advance up to 90% of the face value of coverage using term or permanent life insurance as a result of an illness or accident that shortened your life expectancy.
Ed Scott stated I do not sell life insurance. I am a tax advisor. And as a tax advisor, I can tell you that the single biggest benefit in the federal tax code is the income tax exemption for life insurance. Life Insurance should be a bedrock of any serious financial, retirement or estate plan, but it is not used nearly enough, even by those advisors who do sell life insurance. For planning purposes here, I refer only to permanent insurance, not term insurance.
Obviously, life insurance provides an income tax-free death benefit and people understand that. But besides the death benefit, here are your five best points for encouraging more people to have life insurance to enhance their long-term financial security.
1. IRAs are bad assets; life insurance is a good asset
Most people have their retirement savings in IRAs and 401(k)s. These are bad assets because they are tax-deferred. The tax will one day have to be paid, creating a growing debt on these retirement savings. The future tax will be paid when the money is needed most, in retirement, and at an unknown, but probably higher tax rate.
This makes these traditional retirement accounts an uncertain and diminishing asset over time. Replacing these accounts over time with permanent life insurance turns these tax-deferred funds into tax-free savings. Clients should begin a program of systematic IRA withdrawals to decrease their IRA balances and plow those funds into permanent life insurance.
This tax will have to be paid anyway beginning at age 70 1/2 and probably at a higher rate on a higher balance. So it's best to deal with this now to have more retirement funds available long-term. The increasing and uncertain tax debt is paid off by paying the tax now at known tax rates, which are at historic lows right now, while income tax-free savings are growing in the permanent insurance policy.
2. Life Insurance is an investment, not an expense
People will say life insurance costs too much. Moving funds either from IRAs or from other accounts to permanent life insurance is not an expense; it's an investment in a better long-term asset. Yes, if the funds are withdrawn from an IRA, there will be a tax to pay, but that tax will have had to be paid at some point anyway, probably at higher tax rates in the future.
Once the funds are in a permanent life insurance policy, they are simply located in a different and far better long-term asset than an IRA or 401(k). The funds in that new location, the life insurance policy, remove not only the tax risk but can also eliminate the stock market risk, depending on how the policy is set up.
That's a big deal in retirement, and something you generally cannot do in a traditional IRA. If you were changing investments, you would not think of that as an expense, so the same applies here.
3. Life insurance has lifetime benefits
People think of life insurance for the death benefit, but most people don't know about the powerful lifetime retirement and tax benefits. Funds in a permanent life insurance policy can double as a retirement savings account, but without the worry about what future tax rates will be.
If these funds are needed in retirement, they are accessible, tax- and penalty-free. That is a big deal because if the funds were in an IRA, distributions would not only be taxable (in a traditional IRA), but that increased income could trigger other so-called "stealth taxes."
These are hidden tax increases in the form of phased-out deductions, tax credits, exemptions, and other benefits as income increases. For example, an income increase from an IRA distribution could cause more Social Security benefits to be taxable or trigger the 3.8 percent additional tax on net investment income from capital gains, interest, and dividends.
Accessing funds from a life insurance policy are tax-free (up to cost-basis, and after that if taken as policy loans against the tax-free death benefit) so they don't increase income. And in fact, the withdrawals keep taxable income and taxes lower in retirement. These are valuable lifetime benefits, in addition to the death benefit.
4. More Control with Life Insurance
IRAs are subject to annual required minimum distributions (RMDs) after age 70 1/2, whether the money is needed or not (Roth IRAs are exempt from lifetime RMDs). This causes forced distributions and additional taxes, though the client may not need or want to withdraw those funds.
These forced withdrawals take control away, while withdrawing from the value in a life insurance policy can be done at any time, or not. Clients are in control of their retirement savings in a life insurance policy.
5. Powerful wealth creation through leverage
Life insurance creates more long-term wealth than any other investment. And because this wealth is income tax-free, it is much more valuable than tax-deferred retirement savings that are at the mercy of future higher tax rates.
It's the leverage that creates wealth. Life insurance is the only investment where one dollar can do the work of many, and the result is guaranteed and tax-free. With an IRA, for example, it would take many years to multiply that balance; and when it is withdrawn, it will be diminished by taxes.
Taking the same funds that were in an IRA and investing them (after-the tax was paid on the IRA distribution) in a permanent life insurance policy, would produce many multiples of that original IRA balance, and it would be tax-free, not only for use during life but especially if there were an early death.
Finding the money to pay for life insurance
1 Stop Benefits is uniquely able to secure life insurance coverage at just about any age. We have individual plans that guaranteed coverage up to $100,000 if you are actively at work or smaller amounts id not able to work regardless of health, weight, or occupation. Of course, it is to your advantage to purchase early or without a pre-existing condition.
Leveraging your bad assets to pay for good assets should be your New Year's resolution. If you have money tied up in none performing stocks, under leverage property, are over 59 1/2, you have sources to pay premiums. Consider the need for cash in the future for long-term care especially if you do not have separate coverage or want to live out your life in your home. Healthcare premiums exceed $20,000 a family! What are some solutions?
Wednesday, October 09, 2019 Craig E. Chapin
 Options to Save On Group Health Insurance
As health premiums increase each year, employers are looking for solutions. Employees struggle to afford both their cost-sharing on premiums plus their out-of-pocket cost for care. The annual MOOP (maximum out-of-pocket) cost is rising to $8,150 per individual and $16,300 per family in 2020. Unfortunately, the savings rate for Americans is decreasing, and most have less than a $1,000 set aside for an emergency. Employer options to reduce costs include changing insurance companies, raising deductibles, reducing network access, or raising employees' contributions. Employers need solutions as the average family cost for health insurance exceeds $20,000 a year.
When discussing solutions, consider the odds of use, the type of service used, and the availability to use tax-saving vehicles or to leverage the risk. Look for plan flexibility and offering employee choice, but always look for wide access to providers. Beware of tiered networks that do not offer nationwide coverage at a higher cost. Ask if prescription cards are necessary, and if a choice of prescription cards can be offered.
Use common sense when designing your group plan. 20% of any group spends 80% of the health care expense. Consider spreading the risk on the entire group to pay the claims experienced by the few. This is a great option for groups that seek quality employee benefits and want to lower the maximum out-of-pocket cost for employees at no additional cost to the company. Watch Video https://www.linkedin.com/pulse/common-sense-health-plans-only-lowers-groups-overall-cost-chapin
Transparency is needed in health care to reduce waste and to seek lower-cost services. I implore everyone to look at their health insurance member portal and check out the difference between billed charges and allowed charges. The night and day differences are staggering, especially for doctors, labs, and emergency room costs. Unfortunately, most people need to incur the cost before we see the difference in contracted charges. Consider using http://www.fairhealthconsumer.org or https://www.newchoicehealth.com/Directory for estimates.
The average cost for each employee to have a prescription card is $150 a month and over $400 per month per family. Specialists, especially in the fields of dermatology and orthopedic medicine, maybe part of the problem as they direct people to the latest and greatest drugs advertised by big pharma. We can also be our worst enemy asking to be put on medications advertised on T.V. and magazines. I spent one weekend writing down the names of brand name medication advertised.
Options to Save On Group Health Insurance
As health premiums increase each year, employers are looking for solutions. Employees struggle to afford both their cost-sharing on premiums plus their out-of-pocket cost for care. The annual MOOP (maximum out-of-pocket) cost is rising to $8,150 per individual and $16,300 per family in 2020. Unfortunately, the savings rate for Americans is decreasing, and most have less than a $1,000 set aside for an emergency. Employer options to reduce costs include changing insurance companies, raising deductibles, reducing network access, or raising employees' contributions. Employers need solutions as the average family cost for health insurance exceeds $20,000 a year.
When discussing solutions, consider the odds of use, the type of service used, and the availability to use tax-saving vehicles or to leverage the risk. Look for plan flexibility and offering employee choice, but always look for wide access to providers. Beware of tiered networks that do not offer nationwide coverage at a higher cost. Ask if prescription cards are necessary, and if a choice of prescription cards can be offered.
Use common sense when designing your group plan. 20% of any group spends 80% of the health care expense. Consider spreading the risk on the entire group to pay the claims experienced by the few. This is a great option for groups that seek quality employee benefits and want to lower the maximum out-of-pocket cost for employees at no additional cost to the company. Watch Video https://www.linkedin.com/pulse/common-sense-health-plans-only-lowers-groups-overall-cost-chapin
Transparency is needed in health care to reduce waste and to seek lower-cost services. I implore everyone to look at their health insurance member portal and check out the difference between billed charges and allowed charges. The night and day differences are staggering, especially for doctors, labs, and emergency room costs. Unfortunately, most people need to incur the cost before we see the difference in contracted charges. Consider using http://www.fairhealthconsumer.org or https://www.newchoicehealth.com/Directory for estimates.
The average cost for each employee to have a prescription card is $150 a month and over $400 per month per family. Specialists, especially in the fields of dermatology and orthopedic medicine, maybe part of the problem as they direct people to the latest and greatest drugs advertised by big pharma. We can also be our worst enemy asking to be put on medications advertised on T.V. and magazines. I spent one weekend writing down the names of brand name medication advertised.
 Offer a choice to your employees on prescription options or no card at all. If the company shares in the cost, consider passing the savings on to the employees in an HRA to cover other expenses, including medical, dental, and vision expenses.
Medicare Part D reported in 2017 that the top 250 medications dispensed equal 77.85 percent of total spending. Eighty-five of the top 250 medications cost over $10,000 per beneficiary. Most people under age 65 take fewer prescriptions then seniors. Eighty-nine percent of all medications dispensed are for generic drugs, and the average generic cost is $18 per fill.
The ACA eliminates the need to show medical evidence to switch plans and benefits at open enrollment, or with a special enrollment event. The risk of needing one of these new types of medication overnight is slight.
PPO/POS plans offer out-of-network coverage versus an EPO/HMO. Do not be fooled into thinking that having out-of-network benefits is better as most of these plan designs reimburse charges at a small percentage over the Medicare allowance. You will be billed for excess charges as no contractual agreement protects you. Closed network plans, using network facilities protect you from paying non-network providers - called surprise billing.
Throughout my three decades in the healthcare industry, and after having raised three children as well as my own fair share of serious surgeries in closed network plans, I have not seen anyone stuck paying non-network providers such as an Anesthesiologist if they took reasonable steps to use the network. Sometimes it takes a little time for the insurance company to haggle on the final price, but the clients have not been held accountable.
Call Craig Chapin 1 Stop Benefits, Inc. 1-800-662-3982 Sales@1StopBenefits.com
Offer a choice to your employees on prescription options or no card at all. If the company shares in the cost, consider passing the savings on to the employees in an HRA to cover other expenses, including medical, dental, and vision expenses.
Medicare Part D reported in 2017 that the top 250 medications dispensed equal 77.85 percent of total spending. Eighty-five of the top 250 medications cost over $10,000 per beneficiary. Most people under age 65 take fewer prescriptions then seniors. Eighty-nine percent of all medications dispensed are for generic drugs, and the average generic cost is $18 per fill.
The ACA eliminates the need to show medical evidence to switch plans and benefits at open enrollment, or with a special enrollment event. The risk of needing one of these new types of medication overnight is slight.
PPO/POS plans offer out-of-network coverage versus an EPO/HMO. Do not be fooled into thinking that having out-of-network benefits is better as most of these plan designs reimburse charges at a small percentage over the Medicare allowance. You will be billed for excess charges as no contractual agreement protects you. Closed network plans, using network facilities protect you from paying non-network providers - called surprise billing.
Throughout my three decades in the healthcare industry, and after having raised three children as well as my own fair share of serious surgeries in closed network plans, I have not seen anyone stuck paying non-network providers such as an Anesthesiologist if they took reasonable steps to use the network. Sometimes it takes a little time for the insurance company to haggle on the final price, but the clients have not been held accountable.
Call Craig Chapin 1 Stop Benefits, Inc. 1-800-662-3982 Sales@1StopBenefits.com
 Options to Save On Group Health Insurance
As health premiums increase each year, employers are looking for solutions. Employees struggle to afford both their cost-sharing on premiums plus their out-of-pocket cost for care. The annual MOOP (maximum out-of-pocket) cost is rising to $8,150 per individual and $16,300 per family in 2020. Unfortunately, the savings rate for Americans is decreasing, and most have less than a $1,000 set aside for an emergency. Employer options to reduce costs include changing insurance companies, raising deductibles, reducing network access, or raising employees' contributions. Employers need solutions as the average family cost for health insurance exceeds $20,000 a year.
When discussing solutions, consider the odds of use, the type of service used, and the availability to use tax-saving vehicles or to leverage the risk. Look for plan flexibility and offering employee choice, but always look for wide access to providers. Beware of tiered networks that do not offer nationwide coverage at a higher cost. Ask if prescription cards are necessary, and if a choice of prescription cards can be offered.
Use common sense when designing your group plan. 20% of any group spends 80% of the health care expense. Consider spreading the risk on the entire group to pay the claims experienced by the few. This is a great option for groups that seek quality employee benefits and want to lower the maximum out-of-pocket cost for employees at no additional cost to the company. Watch Video https://www.linkedin.com/pulse/common-sense-health-plans-only-lowers-groups-overall-cost-chapin
Transparency is needed in health care to reduce waste and to seek lower-cost services. I implore everyone to look at their health insurance member portal and check out the difference between billed charges and allowed charges. The night and day differences are staggering, especially for doctors, labs, and emergency room costs. Unfortunately, most people need to incur the cost before we see the difference in contracted charges. Consider using http://www.fairhealthconsumer.org or https://www.newchoicehealth.com/Directory for estimates.
The average cost for each employee to have a prescription card is $150 a month and over $400 per month per family. Specialists, especially in the fields of dermatology and orthopedic medicine, maybe part of the problem as they direct people to the latest and greatest drugs advertised by big pharma. We can also be our worst enemy asking to be put on medications advertised on T.V. and magazines. I spent one weekend writing down the names of brand name medication advertised.
Options to Save On Group Health Insurance
As health premiums increase each year, employers are looking for solutions. Employees struggle to afford both their cost-sharing on premiums plus their out-of-pocket cost for care. The annual MOOP (maximum out-of-pocket) cost is rising to $8,150 per individual and $16,300 per family in 2020. Unfortunately, the savings rate for Americans is decreasing, and most have less than a $1,000 set aside for an emergency. Employer options to reduce costs include changing insurance companies, raising deductibles, reducing network access, or raising employees' contributions. Employers need solutions as the average family cost for health insurance exceeds $20,000 a year.
When discussing solutions, consider the odds of use, the type of service used, and the availability to use tax-saving vehicles or to leverage the risk. Look for plan flexibility and offering employee choice, but always look for wide access to providers. Beware of tiered networks that do not offer nationwide coverage at a higher cost. Ask if prescription cards are necessary, and if a choice of prescription cards can be offered.
Use common sense when designing your group plan. 20% of any group spends 80% of the health care expense. Consider spreading the risk on the entire group to pay the claims experienced by the few. This is a great option for groups that seek quality employee benefits and want to lower the maximum out-of-pocket cost for employees at no additional cost to the company. Watch Video https://www.linkedin.com/pulse/common-sense-health-plans-only-lowers-groups-overall-cost-chapin
Transparency is needed in health care to reduce waste and to seek lower-cost services. I implore everyone to look at their health insurance member portal and check out the difference between billed charges and allowed charges. The night and day differences are staggering, especially for doctors, labs, and emergency room costs. Unfortunately, most people need to incur the cost before we see the difference in contracted charges. Consider using http://www.fairhealthconsumer.org or https://www.newchoicehealth.com/Directory for estimates.
The average cost for each employee to have a prescription card is $150 a month and over $400 per month per family. Specialists, especially in the fields of dermatology and orthopedic medicine, maybe part of the problem as they direct people to the latest and greatest drugs advertised by big pharma. We can also be our worst enemy asking to be put on medications advertised on T.V. and magazines. I spent one weekend writing down the names of brand name medication advertised.
 Offer a choice to your employees on prescription options or no card at all. If the company shares in the cost, consider passing the savings on to the employees in an HRA to cover other expenses, including medical, dental, and vision expenses.
Medicare Part D reported in 2017 that the top 250 medications dispensed equal 77.85 percent of total spending. Eighty-five of the top 250 medications cost over $10,000 per beneficiary. Most people under age 65 take fewer prescriptions then seniors. Eighty-nine percent of all medications dispensed are for generic drugs, and the average generic cost is $18 per fill.
The ACA eliminates the need to show medical evidence to switch plans and benefits at open enrollment, or with a special enrollment event. The risk of needing one of these new types of medication overnight is slight.
PPO/POS plans offer out-of-network coverage versus an EPO/HMO. Do not be fooled into thinking that having out-of-network benefits is better as most of these plan designs reimburse charges at a small percentage over the Medicare allowance. You will be billed for excess charges as no contractual agreement protects you. Closed network plans, using network facilities protect you from paying non-network providers - called surprise billing.
Throughout my three decades in the healthcare industry, and after having raised three children as well as my own fair share of serious surgeries in closed network plans, I have not seen anyone stuck paying non-network providers such as an Anesthesiologist if they took reasonable steps to use the network. Sometimes it takes a little time for the insurance company to haggle on the final price, but the clients have not been held accountable.
Call Craig Chapin 1 Stop Benefits, Inc. 1-800-662-3982 Sales@1StopBenefits.com
Offer a choice to your employees on prescription options or no card at all. If the company shares in the cost, consider passing the savings on to the employees in an HRA to cover other expenses, including medical, dental, and vision expenses.
Medicare Part D reported in 2017 that the top 250 medications dispensed equal 77.85 percent of total spending. Eighty-five of the top 250 medications cost over $10,000 per beneficiary. Most people under age 65 take fewer prescriptions then seniors. Eighty-nine percent of all medications dispensed are for generic drugs, and the average generic cost is $18 per fill.
The ACA eliminates the need to show medical evidence to switch plans and benefits at open enrollment, or with a special enrollment event. The risk of needing one of these new types of medication overnight is slight.
PPO/POS plans offer out-of-network coverage versus an EPO/HMO. Do not be fooled into thinking that having out-of-network benefits is better as most of these plan designs reimburse charges at a small percentage over the Medicare allowance. You will be billed for excess charges as no contractual agreement protects you. Closed network plans, using network facilities protect you from paying non-network providers - called surprise billing.
Throughout my three decades in the healthcare industry, and after having raised three children as well as my own fair share of serious surgeries in closed network plans, I have not seen anyone stuck paying non-network providers such as an Anesthesiologist if they took reasonable steps to use the network. Sometimes it takes a little time for the insurance company to haggle on the final price, but the clients have not been held accountable.
Call Craig Chapin 1 Stop Benefits, Inc. 1-800-662-3982 Sales@1StopBenefits.com
Flexibility added to the ICHRA addressing affordability and access to individual Federal subsidies.
Friday, August 02, 2019 By Caitlin Bronson People Keep
 Employees participating in an individual coverage HRA (ICHRA) cannot collect premium tax credits. However, the federal government added some flexibility to the ICHRA rules.
With an ICHRA, employees have a choice: they can either participate in the HRA and waive their right to premium tax credits, or they can opt out of the ICHRA and (if qualified) collect their premium tax credits.
In this post, we'll go over what the ICHRA regulations say about premium tax credits, how premium tax credits are affected by ICHRA availability, and what employees must do to opt in or out of the benefit.
Let's get started.
What do the ICHRA regulations say?
The ICHRA regulations are clear in their handling of premium tax credits. On page 18 of the final rule, the Departments of the Treasury, Labor, and Health and Human Services state:
An individual is ineligible for the premium tax credit (PTC) for the individual's Exchange coverage for a month if the individual is covered by an HRA or is eligible for an HRA that is affordable and provides minimum value (MV) for the month.
In plainer words, an employee (or any member of the employee's family) can't collect premium tax credits if they participate in the ICHRA.
The regulations offer employees a choice, though. They can opt out of the ICHRA and collect their premium tax credits, provided the benefit qualifies as "unaffordable" under the definition laid out in the Affordable Care Act (ACA). The Departments state:
An employee and a related HRA individual offered an individual coverage HRA that is not affordable will be eligible for the PTC (assuming they are otherwise eligible) if the employee opts out of the individual coverage HRA.
The regulations state that employees must be allowed to make the decision to opt out annually, and must make their decision before the ICHRA plan start date.
Now, let's explore what these guidelines look like in practice.
Calculating affordability with an ICHRA
For employees who qualify for premium tax credits, the most important step in deciding whether or not to participate in the ICHRA is determining if the ICHRA benefit is "affordable."
If the ICHRA is affordable, employees cannot collect tax credits by opting out of it. If the ICHRA is unaffordable, though, they can choose to opt out and use those credits.
The Departments state that an ICHRA is considered affordable if the employee's required HRA contribution for the month is less than 1/12 of the employee's household income for the taxable year multiplied by the required contribution percentage.
The employee's required HRA contribution is determined by the difference between the premium of the lowest cost silver-level plan available on the local exchange and the company's allowance for single employees.
The required contribution percentage, meanwhile, is adjusted annually. For the 2019 plan year, it is 9.86 percent.
Let's look at an example.
Colin is an employee with Brower Construction Company, which pays him $60,000 a year. Brower Construction plans to offer an ICHRA for its employees with a monthly allowance of $100 for single employees. Colin would otherwise qualify for premium tax credits, so he must decide if the allowance is considered affordable or unaffordable.
The lowest cost silver-level plan available on the exchange in Colin's area is $400 a month, which means employees' required HRA contribution with this benefit is $300. One-twelfth of Colin's income for the year is $5,000; multiplied by 9.86 percent, the figure is roughly $493.
Because $493 is more than the required HRA contribution of $300, Colin's ICHRA benefit is considered affordable. This means that he cannot waive the benefit and collect his premium tax credits.
Wayne is another Brower Construction Company employee who qualifies for premium tax credits. Together, he and his wife earn $30,000 a year. One-twelfth of his income is $2,500; multiplied by 9.86 percent, the figure is about $246. Because $246 is less than the required HRA contribution of $300, Wayne's ICHRA benefit is not considered affordable. That means he can waive ICHRA participation and collect his premium tax credits instead.
For purposes of this calculation, the ICHRA regulations state that employees must calculate roughly what they expect to earn on a monthly basis through the taxable year.
They must then choose to keep or waive the ICHRA before the benefit plan year begins.
Waiving premium tax credits in favor of the ICHRA
Employees who are otherwise eligible for premium tax credits may choose to waive access to those credits and participate in the ICHRA.
There are no formal requirements for employees who choose this path. Simply by choosing to participate in the ICHRA, employees are waiving their rights to premium tax credits.
Employees can reevaluate their choice and choose to opt out of the ICHRA in advance of the next plan year, but they can't opt out midyear and then collect premium tax credits.
In our example above, Colin would take this path.
Opting out of the ICHRA in favor of premium tax credits
Employees whose ICHRA benefit is unaffordable may want to opt out of the ICHRA and collect premium tax credits instead. To do this, they must inform their company before the ICHRA plan start date. This choice applies to both the employee and their family.
Once they opt out of the ICHRA, they're free to collect their premium tax credits without any qualification.
Employees can reevaluate their choice and choose to participate in the ICHRA during the next plan year, but once they've chosen to opt out, they can't participate for the rest of that plan year.
In our example above, Wayne would take this path on behalf of himself and his wife.
Premium tax credits and the ICHRA notice requirement
Premium tax credit availability is one of the most important considerations employees must make with regard to the ICHRA. Recognizing that, the federal government requires that employers offering an ICHRA send employees a notice about the benefit that explains how the ICHRA affects premium tax credits.
The ICHRA notice covers many items, but its primary purpose is to help educate employees about their options regarding premium tax credits.
Employers should be ready to fulfill this requirement and offer any help their workers may need.
You can find sample notice language concerning premium tax credits in this FAQ document released by the IRS.
Conclusion
With the ICHRA, the federal government has offered some much-appreciated flexibility when it comes to premium tax credits. Employees can examine their personal circumstances, determine the best route for their family, and either opt in or opt out of the benefit.
State and federal exchanges should be working to help employees determine ICHRA affordability in 2020, but employers should be ready to help make the calculation as simple as possible through materials like the ICHRA notice.
Employees participating in an individual coverage HRA (ICHRA) cannot collect premium tax credits. However, the federal government added some flexibility to the ICHRA rules.
With an ICHRA, employees have a choice: they can either participate in the HRA and waive their right to premium tax credits, or they can opt out of the ICHRA and (if qualified) collect their premium tax credits.
In this post, we'll go over what the ICHRA regulations say about premium tax credits, how premium tax credits are affected by ICHRA availability, and what employees must do to opt in or out of the benefit.
Let's get started.
What do the ICHRA regulations say?
The ICHRA regulations are clear in their handling of premium tax credits. On page 18 of the final rule, the Departments of the Treasury, Labor, and Health and Human Services state:
An individual is ineligible for the premium tax credit (PTC) for the individual's Exchange coverage for a month if the individual is covered by an HRA or is eligible for an HRA that is affordable and provides minimum value (MV) for the month.
In plainer words, an employee (or any member of the employee's family) can't collect premium tax credits if they participate in the ICHRA.
The regulations offer employees a choice, though. They can opt out of the ICHRA and collect their premium tax credits, provided the benefit qualifies as "unaffordable" under the definition laid out in the Affordable Care Act (ACA). The Departments state:
An employee and a related HRA individual offered an individual coverage HRA that is not affordable will be eligible for the PTC (assuming they are otherwise eligible) if the employee opts out of the individual coverage HRA.
The regulations state that employees must be allowed to make the decision to opt out annually, and must make their decision before the ICHRA plan start date.
Now, let's explore what these guidelines look like in practice.
Calculating affordability with an ICHRA
For employees who qualify for premium tax credits, the most important step in deciding whether or not to participate in the ICHRA is determining if the ICHRA benefit is "affordable."
If the ICHRA is affordable, employees cannot collect tax credits by opting out of it. If the ICHRA is unaffordable, though, they can choose to opt out and use those credits.
The Departments state that an ICHRA is considered affordable if the employee's required HRA contribution for the month is less than 1/12 of the employee's household income for the taxable year multiplied by the required contribution percentage.
The employee's required HRA contribution is determined by the difference between the premium of the lowest cost silver-level plan available on the local exchange and the company's allowance for single employees.
The required contribution percentage, meanwhile, is adjusted annually. For the 2019 plan year, it is 9.86 percent.
Let's look at an example.
Colin is an employee with Brower Construction Company, which pays him $60,000 a year. Brower Construction plans to offer an ICHRA for its employees with a monthly allowance of $100 for single employees. Colin would otherwise qualify for premium tax credits, so he must decide if the allowance is considered affordable or unaffordable.
The lowest cost silver-level plan available on the exchange in Colin's area is $400 a month, which means employees' required HRA contribution with this benefit is $300. One-twelfth of Colin's income for the year is $5,000; multiplied by 9.86 percent, the figure is roughly $493.
Because $493 is more than the required HRA contribution of $300, Colin's ICHRA benefit is considered affordable. This means that he cannot waive the benefit and collect his premium tax credits.
Wayne is another Brower Construction Company employee who qualifies for premium tax credits. Together, he and his wife earn $30,000 a year. One-twelfth of his income is $2,500; multiplied by 9.86 percent, the figure is about $246. Because $246 is less than the required HRA contribution of $300, Wayne's ICHRA benefit is not considered affordable. That means he can waive ICHRA participation and collect his premium tax credits instead.
For purposes of this calculation, the ICHRA regulations state that employees must calculate roughly what they expect to earn on a monthly basis through the taxable year.
They must then choose to keep or waive the ICHRA before the benefit plan year begins.
Waiving premium tax credits in favor of the ICHRA
Employees who are otherwise eligible for premium tax credits may choose to waive access to those credits and participate in the ICHRA.
There are no formal requirements for employees who choose this path. Simply by choosing to participate in the ICHRA, employees are waiving their rights to premium tax credits.
Employees can reevaluate their choice and choose to opt out of the ICHRA in advance of the next plan year, but they can't opt out midyear and then collect premium tax credits.
In our example above, Colin would take this path.
Opting out of the ICHRA in favor of premium tax credits
Employees whose ICHRA benefit is unaffordable may want to opt out of the ICHRA and collect premium tax credits instead. To do this, they must inform their company before the ICHRA plan start date. This choice applies to both the employee and their family.
Once they opt out of the ICHRA, they're free to collect their premium tax credits without any qualification.
Employees can reevaluate their choice and choose to participate in the ICHRA during the next plan year, but once they've chosen to opt out, they can't participate for the rest of that plan year.
In our example above, Wayne would take this path on behalf of himself and his wife.
Premium tax credits and the ICHRA notice requirement
Premium tax credit availability is one of the most important considerations employees must make with regard to the ICHRA. Recognizing that, the federal government requires that employers offering an ICHRA send employees a notice about the benefit that explains how the ICHRA affects premium tax credits.
The ICHRA notice covers many items, but its primary purpose is to help educate employees about their options regarding premium tax credits.
Employers should be ready to fulfill this requirement and offer any help their workers may need.
You can find sample notice language concerning premium tax credits in this FAQ document released by the IRS.
Conclusion
With the ICHRA, the federal government has offered some much-appreciated flexibility when it comes to premium tax credits. Employees can examine their personal circumstances, determine the best route for their family, and either opt in or opt out of the benefit.
State and federal exchanges should be working to help employees determine ICHRA affordability in 2020, but employers should be ready to help make the calculation as simple as possible through materials like the ICHRA notice.
 Employees participating in an individual coverage HRA (ICHRA) cannot collect premium tax credits. However, the federal government added some flexibility to the ICHRA rules.
With an ICHRA, employees have a choice: they can either participate in the HRA and waive their right to premium tax credits, or they can opt out of the ICHRA and (if qualified) collect their premium tax credits.
In this post, we'll go over what the ICHRA regulations say about premium tax credits, how premium tax credits are affected by ICHRA availability, and what employees must do to opt in or out of the benefit.
Let's get started.
What do the ICHRA regulations say?
The ICHRA regulations are clear in their handling of premium tax credits. On page 18 of the final rule, the Departments of the Treasury, Labor, and Health and Human Services state:
An individual is ineligible for the premium tax credit (PTC) for the individual's Exchange coverage for a month if the individual is covered by an HRA or is eligible for an HRA that is affordable and provides minimum value (MV) for the month.
In plainer words, an employee (or any member of the employee's family) can't collect premium tax credits if they participate in the ICHRA.
The regulations offer employees a choice, though. They can opt out of the ICHRA and collect their premium tax credits, provided the benefit qualifies as "unaffordable" under the definition laid out in the Affordable Care Act (ACA). The Departments state:
An employee and a related HRA individual offered an individual coverage HRA that is not affordable will be eligible for the PTC (assuming they are otherwise eligible) if the employee opts out of the individual coverage HRA.
The regulations state that employees must be allowed to make the decision to opt out annually, and must make their decision before the ICHRA plan start date.
Now, let's explore what these guidelines look like in practice.
Calculating affordability with an ICHRA
For employees who qualify for premium tax credits, the most important step in deciding whether or not to participate in the ICHRA is determining if the ICHRA benefit is "affordable."
If the ICHRA is affordable, employees cannot collect tax credits by opting out of it. If the ICHRA is unaffordable, though, they can choose to opt out and use those credits.
The Departments state that an ICHRA is considered affordable if the employee's required HRA contribution for the month is less than 1/12 of the employee's household income for the taxable year multiplied by the required contribution percentage.
The employee's required HRA contribution is determined by the difference between the premium of the lowest cost silver-level plan available on the local exchange and the company's allowance for single employees.
The required contribution percentage, meanwhile, is adjusted annually. For the 2019 plan year, it is 9.86 percent.
Let's look at an example.
Colin is an employee with Brower Construction Company, which pays him $60,000 a year. Brower Construction plans to offer an ICHRA for its employees with a monthly allowance of $100 for single employees. Colin would otherwise qualify for premium tax credits, so he must decide if the allowance is considered affordable or unaffordable.
The lowest cost silver-level plan available on the exchange in Colin's area is $400 a month, which means employees' required HRA contribution with this benefit is $300. One-twelfth of Colin's income for the year is $5,000; multiplied by 9.86 percent, the figure is roughly $493.
Because $493 is more than the required HRA contribution of $300, Colin's ICHRA benefit is considered affordable. This means that he cannot waive the benefit and collect his premium tax credits.
Wayne is another Brower Construction Company employee who qualifies for premium tax credits. Together, he and his wife earn $30,000 a year. One-twelfth of his income is $2,500; multiplied by 9.86 percent, the figure is about $246. Because $246 is less than the required HRA contribution of $300, Wayne's ICHRA benefit is not considered affordable. That means he can waive ICHRA participation and collect his premium tax credits instead.
For purposes of this calculation, the ICHRA regulations state that employees must calculate roughly what they expect to earn on a monthly basis through the taxable year.
They must then choose to keep or waive the ICHRA before the benefit plan year begins.
Waiving premium tax credits in favor of the ICHRA
Employees who are otherwise eligible for premium tax credits may choose to waive access to those credits and participate in the ICHRA.
There are no formal requirements for employees who choose this path. Simply by choosing to participate in the ICHRA, employees are waiving their rights to premium tax credits.
Employees can reevaluate their choice and choose to opt out of the ICHRA in advance of the next plan year, but they can't opt out midyear and then collect premium tax credits.
In our example above, Colin would take this path.
Opting out of the ICHRA in favor of premium tax credits
Employees whose ICHRA benefit is unaffordable may want to opt out of the ICHRA and collect premium tax credits instead. To do this, they must inform their company before the ICHRA plan start date. This choice applies to both the employee and their family.
Once they opt out of the ICHRA, they're free to collect their premium tax credits without any qualification.
Employees can reevaluate their choice and choose to participate in the ICHRA during the next plan year, but once they've chosen to opt out, they can't participate for the rest of that plan year.
In our example above, Wayne would take this path on behalf of himself and his wife.
Premium tax credits and the ICHRA notice requirement
Premium tax credit availability is one of the most important considerations employees must make with regard to the ICHRA. Recognizing that, the federal government requires that employers offering an ICHRA send employees a notice about the benefit that explains how the ICHRA affects premium tax credits.
The ICHRA notice covers many items, but its primary purpose is to help educate employees about their options regarding premium tax credits.
Employers should be ready to fulfill this requirement and offer any help their workers may need.
You can find sample notice language concerning premium tax credits in this FAQ document released by the IRS.
Conclusion
With the ICHRA, the federal government has offered some much-appreciated flexibility when it comes to premium tax credits. Employees can examine their personal circumstances, determine the best route for their family, and either opt in or opt out of the benefit.
State and federal exchanges should be working to help employees determine ICHRA affordability in 2020, but employers should be ready to help make the calculation as simple as possible through materials like the ICHRA notice.
Employees participating in an individual coverage HRA (ICHRA) cannot collect premium tax credits. However, the federal government added some flexibility to the ICHRA rules.
With an ICHRA, employees have a choice: they can either participate in the HRA and waive their right to premium tax credits, or they can opt out of the ICHRA and (if qualified) collect their premium tax credits.
In this post, we'll go over what the ICHRA regulations say about premium tax credits, how premium tax credits are affected by ICHRA availability, and what employees must do to opt in or out of the benefit.
Let's get started.
What do the ICHRA regulations say?
The ICHRA regulations are clear in their handling of premium tax credits. On page 18 of the final rule, the Departments of the Treasury, Labor, and Health and Human Services state:
An individual is ineligible for the premium tax credit (PTC) for the individual's Exchange coverage for a month if the individual is covered by an HRA or is eligible for an HRA that is affordable and provides minimum value (MV) for the month.
In plainer words, an employee (or any member of the employee's family) can't collect premium tax credits if they participate in the ICHRA.
The regulations offer employees a choice, though. They can opt out of the ICHRA and collect their premium tax credits, provided the benefit qualifies as "unaffordable" under the definition laid out in the Affordable Care Act (ACA). The Departments state:
An employee and a related HRA individual offered an individual coverage HRA that is not affordable will be eligible for the PTC (assuming they are otherwise eligible) if the employee opts out of the individual coverage HRA.
The regulations state that employees must be allowed to make the decision to opt out annually, and must make their decision before the ICHRA plan start date.
Now, let's explore what these guidelines look like in practice.
Calculating affordability with an ICHRA
For employees who qualify for premium tax credits, the most important step in deciding whether or not to participate in the ICHRA is determining if the ICHRA benefit is "affordable."
If the ICHRA is affordable, employees cannot collect tax credits by opting out of it. If the ICHRA is unaffordable, though, they can choose to opt out and use those credits.
The Departments state that an ICHRA is considered affordable if the employee's required HRA contribution for the month is less than 1/12 of the employee's household income for the taxable year multiplied by the required contribution percentage.
The employee's required HRA contribution is determined by the difference between the premium of the lowest cost silver-level plan available on the local exchange and the company's allowance for single employees.
The required contribution percentage, meanwhile, is adjusted annually. For the 2019 plan year, it is 9.86 percent.
Let's look at an example.
Colin is an employee with Brower Construction Company, which pays him $60,000 a year. Brower Construction plans to offer an ICHRA for its employees with a monthly allowance of $100 for single employees. Colin would otherwise qualify for premium tax credits, so he must decide if the allowance is considered affordable or unaffordable.
The lowest cost silver-level plan available on the exchange in Colin's area is $400 a month, which means employees' required HRA contribution with this benefit is $300. One-twelfth of Colin's income for the year is $5,000; multiplied by 9.86 percent, the figure is roughly $493.
Because $493 is more than the required HRA contribution of $300, Colin's ICHRA benefit is considered affordable. This means that he cannot waive the benefit and collect his premium tax credits.
Wayne is another Brower Construction Company employee who qualifies for premium tax credits. Together, he and his wife earn $30,000 a year. One-twelfth of his income is $2,500; multiplied by 9.86 percent, the figure is about $246. Because $246 is less than the required HRA contribution of $300, Wayne's ICHRA benefit is not considered affordable. That means he can waive ICHRA participation and collect his premium tax credits instead.
For purposes of this calculation, the ICHRA regulations state that employees must calculate roughly what they expect to earn on a monthly basis through the taxable year.
They must then choose to keep or waive the ICHRA before the benefit plan year begins.
Waiving premium tax credits in favor of the ICHRA
Employees who are otherwise eligible for premium tax credits may choose to waive access to those credits and participate in the ICHRA.
There are no formal requirements for employees who choose this path. Simply by choosing to participate in the ICHRA, employees are waiving their rights to premium tax credits.
Employees can reevaluate their choice and choose to opt out of the ICHRA in advance of the next plan year, but they can't opt out midyear and then collect premium tax credits.
In our example above, Colin would take this path.
Opting out of the ICHRA in favor of premium tax credits
Employees whose ICHRA benefit is unaffordable may want to opt out of the ICHRA and collect premium tax credits instead. To do this, they must inform their company before the ICHRA plan start date. This choice applies to both the employee and their family.
Once they opt out of the ICHRA, they're free to collect their premium tax credits without any qualification.
Employees can reevaluate their choice and choose to participate in the ICHRA during the next plan year, but once they've chosen to opt out, they can't participate for the rest of that plan year.
In our example above, Wayne would take this path on behalf of himself and his wife.
Premium tax credits and the ICHRA notice requirement
Premium tax credit availability is one of the most important considerations employees must make with regard to the ICHRA. Recognizing that, the federal government requires that employers offering an ICHRA send employees a notice about the benefit that explains how the ICHRA affects premium tax credits.
The ICHRA notice covers many items, but its primary purpose is to help educate employees about their options regarding premium tax credits.
Employers should be ready to fulfill this requirement and offer any help their workers may need.
You can find sample notice language concerning premium tax credits in this FAQ document released by the IRS.
Conclusion
With the ICHRA, the federal government has offered some much-appreciated flexibility when it comes to premium tax credits. Employees can examine their personal circumstances, determine the best route for their family, and either opt in or opt out of the benefit.
State and federal exchanges should be working to help employees determine ICHRA affordability in 2020, but employers should be ready to help make the calculation as simple as possible through materials like the ICHRA notice.Common Sense Health Plans are superior to Level Funding.
Monday, July 08, 2019 Craig E. Chapin
 * 100% of savings are retained by the employer;
* Premiums are not affected by medical conditions;
* All state benefit mandates are included;
* Can be used with ICHRA and extended benefit plans;
* National networks of doctors and hospitals;
* Employee's individual choice of prescription plans;
* No tiered hospital or doctor financial penalties;
* First dollar benefit plan designs;
* Lower MOOP per person, max two per family.
History has shown that twenty percent of employees in any group use eighty percent of the health care dollars. With the Common Sense program, we use a fully insured high deductible insurance plan that pays all preventative care expenses and covers all claims over the MOOP. The basis of all insurance is charging premiums on the many to pay the financial risk of the few.
Today, the ACA does not allow insurance companies offering fully insured plans to ask medical questions or to have pre-existing condition limitations. Insurance companies pass through all negotiated discounts on expenses but assume everyone is a high-end spender of healthcare. Here lies the opportunity.
A level-funded plan includes all claims for preventative care and has a much higher stop loss, typically $25,000 per person. A small employer with just one person having a hospital stay will wipe out any claim reserves that generate the savings for a group. Level funding carrier's cherry pick new customers by analyzing each participant's medical conditions and prescription use.
At One Stop Benefits, we customize Common Sense health programs. You have a blank canvas for plan design. We discuss plan designs that promote shopping for lower cost services and enable employees to estimate what a procedure or medication will cost before services are rendered. The cost for preventative care is covered, the discounts are passed through with a high deductible plan and company funding of the claims before the MOOP kicks in is limited by the employee cost sharing. Plans with co-insurance have a more significant impact on changing usage and employee behavior than a higher co-pay. Plans with a corridor deductible will have a more favorable employee perception and lowering the MOOP will make your health plan more affordable without adding to the companies cost.
Call right now and I will customize your group savings and answer all your questions. Let's create the perfect plan designed to stop the rising cost of health insurance.
* 100% of savings are retained by the employer;
* Premiums are not affected by medical conditions;
* All state benefit mandates are included;
* Can be used with ICHRA and extended benefit plans;
* National networks of doctors and hospitals;
* Employee's individual choice of prescription plans;
* No tiered hospital or doctor financial penalties;
* First dollar benefit plan designs;
* Lower MOOP per person, max two per family.
History has shown that twenty percent of employees in any group use eighty percent of the health care dollars. With the Common Sense program, we use a fully insured high deductible insurance plan that pays all preventative care expenses and covers all claims over the MOOP. The basis of all insurance is charging premiums on the many to pay the financial risk of the few.
Today, the ACA does not allow insurance companies offering fully insured plans to ask medical questions or to have pre-existing condition limitations. Insurance companies pass through all negotiated discounts on expenses but assume everyone is a high-end spender of healthcare. Here lies the opportunity.
A level-funded plan includes all claims for preventative care and has a much higher stop loss, typically $25,000 per person. A small employer with just one person having a hospital stay will wipe out any claim reserves that generate the savings for a group. Level funding carrier's cherry pick new customers by analyzing each participant's medical conditions and prescription use.
At One Stop Benefits, we customize Common Sense health programs. You have a blank canvas for plan design. We discuss plan designs that promote shopping for lower cost services and enable employees to estimate what a procedure or medication will cost before services are rendered. The cost for preventative care is covered, the discounts are passed through with a high deductible plan and company funding of the claims before the MOOP kicks in is limited by the employee cost sharing. Plans with co-insurance have a more significant impact on changing usage and employee behavior than a higher co-pay. Plans with a corridor deductible will have a more favorable employee perception and lowering the MOOP will make your health plan more affordable without adding to the companies cost.
Call right now and I will customize your group savings and answer all your questions. Let's create the perfect plan designed to stop the rising cost of health insurance.
 * 100% of savings are retained by the employer;
* Premiums are not affected by medical conditions;
* All state benefit mandates are included;
* Can be used with ICHRA and extended benefit plans;
* National networks of doctors and hospitals;
* Employee's individual choice of prescription plans;
* No tiered hospital or doctor financial penalties;
* First dollar benefit plan designs;
* Lower MOOP per person, max two per family.
History has shown that twenty percent of employees in any group use eighty percent of the health care dollars. With the Common Sense program, we use a fully insured high deductible insurance plan that pays all preventative care expenses and covers all claims over the MOOP. The basis of all insurance is charging premiums on the many to pay the financial risk of the few.
Today, the ACA does not allow insurance companies offering fully insured plans to ask medical questions or to have pre-existing condition limitations. Insurance companies pass through all negotiated discounts on expenses but assume everyone is a high-end spender of healthcare. Here lies the opportunity.
A level-funded plan includes all claims for preventative care and has a much higher stop loss, typically $25,000 per person. A small employer with just one person having a hospital stay will wipe out any claim reserves that generate the savings for a group. Level funding carrier's cherry pick new customers by analyzing each participant's medical conditions and prescription use.
At One Stop Benefits, we customize Common Sense health programs. You have a blank canvas for plan design. We discuss plan designs that promote shopping for lower cost services and enable employees to estimate what a procedure or medication will cost before services are rendered. The cost for preventative care is covered, the discounts are passed through with a high deductible plan and company funding of the claims before the MOOP kicks in is limited by the employee cost sharing. Plans with co-insurance have a more significant impact on changing usage and employee behavior than a higher co-pay. Plans with a corridor deductible will have a more favorable employee perception and lowering the MOOP will make your health plan more affordable without adding to the companies cost.
Call right now and I will customize your group savings and answer all your questions. Let's create the perfect plan designed to stop the rising cost of health insurance.
* 100% of savings are retained by the employer;
* Premiums are not affected by medical conditions;
* All state benefit mandates are included;
* Can be used with ICHRA and extended benefit plans;
* National networks of doctors and hospitals;
* Employee's individual choice of prescription plans;
* No tiered hospital or doctor financial penalties;
* First dollar benefit plan designs;
* Lower MOOP per person, max two per family.
History has shown that twenty percent of employees in any group use eighty percent of the health care dollars. With the Common Sense program, we use a fully insured high deductible insurance plan that pays all preventative care expenses and covers all claims over the MOOP. The basis of all insurance is charging premiums on the many to pay the financial risk of the few.
Today, the ACA does not allow insurance companies offering fully insured plans to ask medical questions or to have pre-existing condition limitations. Insurance companies pass through all negotiated discounts on expenses but assume everyone is a high-end spender of healthcare. Here lies the opportunity.
A level-funded plan includes all claims for preventative care and has a much higher stop loss, typically $25,000 per person. A small employer with just one person having a hospital stay will wipe out any claim reserves that generate the savings for a group. Level funding carrier's cherry pick new customers by analyzing each participant's medical conditions and prescription use.
At One Stop Benefits, we customize Common Sense health programs. You have a blank canvas for plan design. We discuss plan designs that promote shopping for lower cost services and enable employees to estimate what a procedure or medication will cost before services are rendered. The cost for preventative care is covered, the discounts are passed through with a high deductible plan and company funding of the claims before the MOOP kicks in is limited by the employee cost sharing. Plans with co-insurance have a more significant impact on changing usage and employee behavior than a higher co-pay. Plans with a corridor deductible will have a more favorable employee perception and lowering the MOOP will make your health plan more affordable without adding to the companies cost.
Call right now and I will customize your group savings and answer all your questions. Let's create the perfect plan designed to stop the rising cost of health insurance.
The ICHRA is now the employer's preferred choice.
Wednesday, July 03, 2019 Craig E. Chapin
 On June 17, 2019, the final rules were published on the Individual Consumer Health Reimbursement Account. This law is a more liberal version of the QSEHRA first introduced in December 2016 before President Obama left the office. The administration felt that allowing employers to fund individual health plans would help protect the market with younger healthy participants.
President Trumps requested expansion to stimulate more employers to offer employees health insurance. Now, employers do not have to comply with group insurance company guidelines.
Offering your employees individual health reimbursements for dental, health, and out-of-pocket medical expenses may be your' best option.
* No minimum group participation or contribution rules;
* Any new employee triggers a special enrollment event;
* No COBRA, ERISA, or Family Leave health benefits;
* Eleven classes of eligibility allow complete customization;
* Provides network access based at an employee's location;
* Grandfather your group plan and add ICHRA benefits to new employee;
* FSA and HSA tax savings plans can still be utilized;
* Employee contributions to cost can be paid with pre-taxed dollars;
* Seasonal, part-time, and Medicare can be funded with complete portability.
The start date for new plans is January 1, 2020, but you should start the discussion making process in the coming weeks. You should provide a 90-day notice to eligible employees making October 1 the cut off date. The flexibility of the options and positive education to staff will assure popularity.
The group insurance market and most consultants are on edge as this law is making a dramatic change to how they conduct business. Learn the details right away from someone that puts customers first before profits.
On June 17, 2019, the final rules were published on the Individual Consumer Health Reimbursement Account. This law is a more liberal version of the QSEHRA first introduced in December 2016 before President Obama left the office. The administration felt that allowing employers to fund individual health plans would help protect the market with younger healthy participants.
President Trumps requested expansion to stimulate more employers to offer employees health insurance. Now, employers do not have to comply with group insurance company guidelines.
Offering your employees individual health reimbursements for dental, health, and out-of-pocket medical expenses may be your' best option.
* No minimum group participation or contribution rules;
* Any new employee triggers a special enrollment event;
* No COBRA, ERISA, or Family Leave health benefits;
* Eleven classes of eligibility allow complete customization;
* Provides network access based at an employee's location;
* Grandfather your group plan and add ICHRA benefits to new employee;
* FSA and HSA tax savings plans can still be utilized;
* Employee contributions to cost can be paid with pre-taxed dollars;
* Seasonal, part-time, and Medicare can be funded with complete portability.
The start date for new plans is January 1, 2020, but you should start the discussion making process in the coming weeks. You should provide a 90-day notice to eligible employees making October 1 the cut off date. The flexibility of the options and positive education to staff will assure popularity.
The group insurance market and most consultants are on edge as this law is making a dramatic change to how they conduct business. Learn the details right away from someone that puts customers first before profits.
 On June 17, 2019, the final rules were published on the Individual Consumer Health Reimbursement Account. This law is a more liberal version of the QSEHRA first introduced in December 2016 before President Obama left the office. The administration felt that allowing employers to fund individual health plans would help protect the market with younger healthy participants.
President Trumps requested expansion to stimulate more employers to offer employees health insurance. Now, employers do not have to comply with group insurance company guidelines.
Offering your employees individual health reimbursements for dental, health, and out-of-pocket medical expenses may be your' best option.
* No minimum group participation or contribution rules;
* Any new employee triggers a special enrollment event;
* No COBRA, ERISA, or Family Leave health benefits;
* Eleven classes of eligibility allow complete customization;
* Provides network access based at an employee's location;
* Grandfather your group plan and add ICHRA benefits to new employee;
* FSA and HSA tax savings plans can still be utilized;
* Employee contributions to cost can be paid with pre-taxed dollars;
* Seasonal, part-time, and Medicare can be funded with complete portability.
The start date for new plans is January 1, 2020, but you should start the discussion making process in the coming weeks. You should provide a 90-day notice to eligible employees making October 1 the cut off date. The flexibility of the options and positive education to staff will assure popularity.
The group insurance market and most consultants are on edge as this law is making a dramatic change to how they conduct business. Learn the details right away from someone that puts customers first before profits.
On June 17, 2019, the final rules were published on the Individual Consumer Health Reimbursement Account. This law is a more liberal version of the QSEHRA first introduced in December 2016 before President Obama left the office. The administration felt that allowing employers to fund individual health plans would help protect the market with younger healthy participants.
President Trumps requested expansion to stimulate more employers to offer employees health insurance. Now, employers do not have to comply with group insurance company guidelines.
Offering your employees individual health reimbursements for dental, health, and out-of-pocket medical expenses may be your' best option.
* No minimum group participation or contribution rules;
* Any new employee triggers a special enrollment event;
* No COBRA, ERISA, or Family Leave health benefits;
* Eleven classes of eligibility allow complete customization;
* Provides network access based at an employee's location;
* Grandfather your group plan and add ICHRA benefits to new employee;
* FSA and HSA tax savings plans can still be utilized;
* Employee contributions to cost can be paid with pre-taxed dollars;
* Seasonal, part-time, and Medicare can be funded with complete portability.
The start date for new plans is January 1, 2020, but you should start the discussion making process in the coming weeks. You should provide a 90-day notice to eligible employees making October 1 the cut off date. The flexibility of the options and positive education to staff will assure popularity.
The group insurance market and most consultants are on edge as this law is making a dramatic change to how they conduct business. Learn the details right away from someone that puts customers first before profits.
The One Stop Benefits Bank Solution
Monday, June 24, 2019 Craig E. Chapin
 Help your employee manage their finances with the Benefits Bank. A survey from Salary Finance reports that American businesses lose half a billion dollar a year because their employees are stressed about personal finances. Monthly and quarterly bills make it tough to be happy when most people live paycheck to paycheck.
Employers need to help since stressed-out workers lose about 23-31 days of productive work days per year and are 2.2 times more likely to hunt for a new job. Lost productivity, turnover can cost your company between 11 to 14 percent of total payroll.
Employees with money worries are
* 3.4 times more likely to suffer from anxiety and panic attacks;
* 4 times more likely to suffer from depression;
* 5.8 times more likely not to be able to finish daily tasks;
* 4.9 times more likely to have lower work quality;
* and 8 times more likely to have sleepless nights.
Anxiety is not limited to the poor, with approximately 40 percent of people making more than $100,000 a year are financially unstable, with less than 3 months of savings.
Allow us to offer your employees the education, and tools to manage their fixed expenses one-time a year. Set up a Benefit Bank and calculate the weekly payments using the 1 Stop Benefits Bank Calculator. Wages can be split using direct deposit between accounts on all fixed expenses. Employees do not have to weekly decide how much to put aside to cover all types of monthly, odd quarterly or annual payments that can be automatically paid each month for free. No credit checks using debit visa cards, and employees maintain complete control on all accounts at no cost.
Auto * Cable * Emergency Fund * Insurance * Phone * Rent * Student Loan * etc.
Let duel income workers direct deposit funds into a benefits bank, pay all fixed expenses automatically, leaving the deposable wages to be paid to their current account. After all, it's tough to be happy when you're prone to depression, panic attacks, sleepless nights, and distractions at work on finances. Credit ratings improve, debts decrease, other pre-tax savings services can be added using the Benefits Bank.
Meetings are just $100, and all setup and calculations tools are only $10 per employee. Call 1-800-662-3982 or email Service@1Stop Benefits.com to set up a meeting.
Help your employee manage their finances with the Benefits Bank. A survey from Salary Finance reports that American businesses lose half a billion dollar a year because their employees are stressed about personal finances. Monthly and quarterly bills make it tough to be happy when most people live paycheck to paycheck.
Employers need to help since stressed-out workers lose about 23-31 days of productive work days per year and are 2.2 times more likely to hunt for a new job. Lost productivity, turnover can cost your company between 11 to 14 percent of total payroll.
Employees with money worries are
* 3.4 times more likely to suffer from anxiety and panic attacks;
* 4 times more likely to suffer from depression;
* 5.8 times more likely not to be able to finish daily tasks;
* 4.9 times more likely to have lower work quality;
* and 8 times more likely to have sleepless nights.
Anxiety is not limited to the poor, with approximately 40 percent of people making more than $100,000 a year are financially unstable, with less than 3 months of savings.
Allow us to offer your employees the education, and tools to manage their fixed expenses one-time a year. Set up a Benefit Bank and calculate the weekly payments using the 1 Stop Benefits Bank Calculator. Wages can be split using direct deposit between accounts on all fixed expenses. Employees do not have to weekly decide how much to put aside to cover all types of monthly, odd quarterly or annual payments that can be automatically paid each month for free. No credit checks using debit visa cards, and employees maintain complete control on all accounts at no cost.
Auto * Cable * Emergency Fund * Insurance * Phone * Rent * Student Loan * etc.
Let duel income workers direct deposit funds into a benefits bank, pay all fixed expenses automatically, leaving the deposable wages to be paid to their current account. After all, it's tough to be happy when you're prone to depression, panic attacks, sleepless nights, and distractions at work on finances. Credit ratings improve, debts decrease, other pre-tax savings services can be added using the Benefits Bank.
Meetings are just $100, and all setup and calculations tools are only $10 per employee. Call 1-800-662-3982 or email Service@1Stop Benefits.com to set up a meeting.
 Help your employee manage their finances with the Benefits Bank. A survey from Salary Finance reports that American businesses lose half a billion dollar a year because their employees are stressed about personal finances. Monthly and quarterly bills make it tough to be happy when most people live paycheck to paycheck.
Employers need to help since stressed-out workers lose about 23-31 days of productive work days per year and are 2.2 times more likely to hunt for a new job. Lost productivity, turnover can cost your company between 11 to 14 percent of total payroll.
Employees with money worries are
* 3.4 times more likely to suffer from anxiety and panic attacks;
* 4 times more likely to suffer from depression;
* 5.8 times more likely not to be able to finish daily tasks;
* 4.9 times more likely to have lower work quality;
* and 8 times more likely to have sleepless nights.
Anxiety is not limited to the poor, with approximately 40 percent of people making more than $100,000 a year are financially unstable, with less than 3 months of savings.
Allow us to offer your employees the education, and tools to manage their fixed expenses one-time a year. Set up a Benefit Bank and calculate the weekly payments using the 1 Stop Benefits Bank Calculator. Wages can be split using direct deposit between accounts on all fixed expenses. Employees do not have to weekly decide how much to put aside to cover all types of monthly, odd quarterly or annual payments that can be automatically paid each month for free. No credit checks using debit visa cards, and employees maintain complete control on all accounts at no cost.
Auto * Cable * Emergency Fund * Insurance * Phone * Rent * Student Loan * etc.
Let duel income workers direct deposit funds into a benefits bank, pay all fixed expenses automatically, leaving the deposable wages to be paid to their current account. After all, it's tough to be happy when you're prone to depression, panic attacks, sleepless nights, and distractions at work on finances. Credit ratings improve, debts decrease, other pre-tax savings services can be added using the Benefits Bank.
Meetings are just $100, and all setup and calculations tools are only $10 per employee. Call 1-800-662-3982 or email Service@1Stop Benefits.com to set up a meeting.
Help your employee manage their finances with the Benefits Bank. A survey from Salary Finance reports that American businesses lose half a billion dollar a year because their employees are stressed about personal finances. Monthly and quarterly bills make it tough to be happy when most people live paycheck to paycheck.
Employers need to help since stressed-out workers lose about 23-31 days of productive work days per year and are 2.2 times more likely to hunt for a new job. Lost productivity, turnover can cost your company between 11 to 14 percent of total payroll.
Employees with money worries are
* 3.4 times more likely to suffer from anxiety and panic attacks;
* 4 times more likely to suffer from depression;
* 5.8 times more likely not to be able to finish daily tasks;
* 4.9 times more likely to have lower work quality;
* and 8 times more likely to have sleepless nights.
Anxiety is not limited to the poor, with approximately 40 percent of people making more than $100,000 a year are financially unstable, with less than 3 months of savings.
Allow us to offer your employees the education, and tools to manage their fixed expenses one-time a year. Set up a Benefit Bank and calculate the weekly payments using the 1 Stop Benefits Bank Calculator. Wages can be split using direct deposit between accounts on all fixed expenses. Employees do not have to weekly decide how much to put aside to cover all types of monthly, odd quarterly or annual payments that can be automatically paid each month for free. No credit checks using debit visa cards, and employees maintain complete control on all accounts at no cost.
Auto * Cable * Emergency Fund * Insurance * Phone * Rent * Student Loan * etc.
Let duel income workers direct deposit funds into a benefits bank, pay all fixed expenses automatically, leaving the deposable wages to be paid to their current account. After all, it's tough to be happy when you're prone to depression, panic attacks, sleepless nights, and distractions at work on finances. Credit ratings improve, debts decrease, other pre-tax savings services can be added using the Benefits Bank.
Meetings are just $100, and all setup and calculations tools are only $10 per employee. Call 1-800-662-3982 or email Service@1Stop Benefits.com to set up a meeting.
Social Security fund to run dry in 2034
Tuesday, April 22, 2019 Nick Thornton
 Social Security is about to pay out more money than it earns for the first time in decades, according to the 2019 OASDI Trustees Report, released today.
By 2020, obligations to retirees and disabled Americans will cost more than Social Security's revenue from payroll taxes, taxes on benefits, and interest earned on investments.
That imbalance is expected to continue until the SSA's main trust fund-the Old-Age and Survivors Insurance fund-is depleted in 2034, at which time scheduled benefits would be cut 23 percent to retirees. This year's projection is inline with last year's Trustees Report.
Social Security's other trust fund-the much smaller Disability Insurance Fund-is in much better shape than previously projected. The DI Fund is now projected to remain solvent to 2052, a 20-year improvement over last year's projection, owed to the continued decline of disability applications since the end of the Great Recession.
Together, OASI and DI funds will be depleted in 2035, a one-year improvement over last year's projection, the report says.
But that headline is potentially misleading. The report notes that under current law, the cuts in scheduled benefits begin separately for each program: 2034 for the OASI program, and 2052 for the DI program.
Last time SS was revenue negative, Congress moved to reform funding
When Social Security begins drawing down its $2.9 trillion in reserves next year, it will be the first time the agency will pay out more than it takes in since 1982.
That underscored the imminent funding issues Social Security was then facing, and spurred amendments that were signed into law in 1983 that included the taxation of some Social Security benefits, an increase in the retirement age, and coverage of federal employees.
Back then, control of Congress was divided as it is today-Democrats controlled the House of Representatives, Republicans controlled the Senate. The amendments were passed with bipartisan support and signed in to law by President Regan.
While Democrats and Republicans have introduced bills to reform Social Security in recent Congressional sessions, and the House Ways and Means Committee held a productive hearing on reform at the outset of the 116th Congress, the parties are at loggerheads over a path to solvency.
Democratic proposals include a phased-in increase of the payroll tax for all Americans, and an expansion of benefits for the most vulnerable Americans. Republican proposals favor raising the retirement age.
As it has in previous years, the Trustees Report urges immediate attention from lawmakers, and warns against the costs of kicking the can down the road.
"The Trustees recommend that lawmakers address the projected trust fund shortfalls in a timely way in order to phase in necessary changes gradually and give workers and beneficiaries time to adjust to them," this year's report says. "Implementing changes sooner rather than later would allow more generations to share in the needed revenue increases or reductions in scheduled benefits."
Social Security's 75-year actuarial deficit is $13.9 trillion. In order for its two funds to remain solvent over that period, payroll taxes would have to be increased by 2.7 percent to 15.1 percent, or benefits would have to be reduced by 17 percent for all current and future beneficiaries, or a combination of each approach could be applied, the report says.
"If actions are deferred for several years, the changes necessary to maintain Social Security solvency become concentrated on fewer years and fewer generations," the Trustees say.
Inside the numbers
An estimated 176 million people had earnings covered by payroll and Social Security taxes in 2018. About 52.7 million people received $845 billion in retirement benefits, and 10.2 million received $143.7 billion in disability payments. Social Security is expected to pay benefits to about 64 million beneficiaries in 2019.
The OASI program took in $715.9 billion in payroll taxes, $34.5 billion in taxes on Social Security benefits, and $80.7 billion in interest payments on invested reserves.
The DI program took in $169.2 billion in payroll taxes, accounting for most of its $25.5 billion surplus in 2018.
Both programs are facing considerable demographic headwinds with the retirement of baby boomers. There were about 2.8 workers for every Social Security beneficiary in 2018.
That ratio was 3.2 to 3.4 between 1974 and 2008. It is expected to continue to decline through 2035, when it will be 2.2 workers per beneficiary, as the baby boomer generation becomes fully retired.
Social Security is about to pay out more money than it earns for the first time in decades, according to the 2019 OASDI Trustees Report, released today.
By 2020, obligations to retirees and disabled Americans will cost more than Social Security's revenue from payroll taxes, taxes on benefits, and interest earned on investments.
That imbalance is expected to continue until the SSA's main trust fund-the Old-Age and Survivors Insurance fund-is depleted in 2034, at which time scheduled benefits would be cut 23 percent to retirees. This year's projection is inline with last year's Trustees Report.
Social Security's other trust fund-the much smaller Disability Insurance Fund-is in much better shape than previously projected. The DI Fund is now projected to remain solvent to 2052, a 20-year improvement over last year's projection, owed to the continued decline of disability applications since the end of the Great Recession.
Together, OASI and DI funds will be depleted in 2035, a one-year improvement over last year's projection, the report says.
But that headline is potentially misleading. The report notes that under current law, the cuts in scheduled benefits begin separately for each program: 2034 for the OASI program, and 2052 for the DI program.
Last time SS was revenue negative, Congress moved to reform funding
When Social Security begins drawing down its $2.9 trillion in reserves next year, it will be the first time the agency will pay out more than it takes in since 1982.
That underscored the imminent funding issues Social Security was then facing, and spurred amendments that were signed into law in 1983 that included the taxation of some Social Security benefits, an increase in the retirement age, and coverage of federal employees.
Back then, control of Congress was divided as it is today-Democrats controlled the House of Representatives, Republicans controlled the Senate. The amendments were passed with bipartisan support and signed in to law by President Regan.
While Democrats and Republicans have introduced bills to reform Social Security in recent Congressional sessions, and the House Ways and Means Committee held a productive hearing on reform at the outset of the 116th Congress, the parties are at loggerheads over a path to solvency.
Democratic proposals include a phased-in increase of the payroll tax for all Americans, and an expansion of benefits for the most vulnerable Americans. Republican proposals favor raising the retirement age.
As it has in previous years, the Trustees Report urges immediate attention from lawmakers, and warns against the costs of kicking the can down the road.
"The Trustees recommend that lawmakers address the projected trust fund shortfalls in a timely way in order to phase in necessary changes gradually and give workers and beneficiaries time to adjust to them," this year's report says. "Implementing changes sooner rather than later would allow more generations to share in the needed revenue increases or reductions in scheduled benefits."
Social Security's 75-year actuarial deficit is $13.9 trillion. In order for its two funds to remain solvent over that period, payroll taxes would have to be increased by 2.7 percent to 15.1 percent, or benefits would have to be reduced by 17 percent for all current and future beneficiaries, or a combination of each approach could be applied, the report says.
"If actions are deferred for several years, the changes necessary to maintain Social Security solvency become concentrated on fewer years and fewer generations," the Trustees say.
Inside the numbers
An estimated 176 million people had earnings covered by payroll and Social Security taxes in 2018. About 52.7 million people received $845 billion in retirement benefits, and 10.2 million received $143.7 billion in disability payments. Social Security is expected to pay benefits to about 64 million beneficiaries in 2019.
The OASI program took in $715.9 billion in payroll taxes, $34.5 billion in taxes on Social Security benefits, and $80.7 billion in interest payments on invested reserves.
The DI program took in $169.2 billion in payroll taxes, accounting for most of its $25.5 billion surplus in 2018.
Both programs are facing considerable demographic headwinds with the retirement of baby boomers. There were about 2.8 workers for every Social Security beneficiary in 2018.
That ratio was 3.2 to 3.4 between 1974 and 2008. It is expected to continue to decline through 2035, when it will be 2.2 workers per beneficiary, as the baby boomer generation becomes fully retired.
 Social Security is about to pay out more money than it earns for the first time in decades, according to the 2019 OASDI Trustees Report, released today.
By 2020, obligations to retirees and disabled Americans will cost more than Social Security's revenue from payroll taxes, taxes on benefits, and interest earned on investments.
That imbalance is expected to continue until the SSA's main trust fund-the Old-Age and Survivors Insurance fund-is depleted in 2034, at which time scheduled benefits would be cut 23 percent to retirees. This year's projection is inline with last year's Trustees Report.
Social Security's other trust fund-the much smaller Disability Insurance Fund-is in much better shape than previously projected. The DI Fund is now projected to remain solvent to 2052, a 20-year improvement over last year's projection, owed to the continued decline of disability applications since the end of the Great Recession.
Together, OASI and DI funds will be depleted in 2035, a one-year improvement over last year's projection, the report says.
But that headline is potentially misleading. The report notes that under current law, the cuts in scheduled benefits begin separately for each program: 2034 for the OASI program, and 2052 for the DI program.
Last time SS was revenue negative, Congress moved to reform funding
When Social Security begins drawing down its $2.9 trillion in reserves next year, it will be the first time the agency will pay out more than it takes in since 1982.
That underscored the imminent funding issues Social Security was then facing, and spurred amendments that were signed into law in 1983 that included the taxation of some Social Security benefits, an increase in the retirement age, and coverage of federal employees.
Back then, control of Congress was divided as it is today-Democrats controlled the House of Representatives, Republicans controlled the Senate. The amendments were passed with bipartisan support and signed in to law by President Regan.
While Democrats and Republicans have introduced bills to reform Social Security in recent Congressional sessions, and the House Ways and Means Committee held a productive hearing on reform at the outset of the 116th Congress, the parties are at loggerheads over a path to solvency.
Democratic proposals include a phased-in increase of the payroll tax for all Americans, and an expansion of benefits for the most vulnerable Americans. Republican proposals favor raising the retirement age.
As it has in previous years, the Trustees Report urges immediate attention from lawmakers, and warns against the costs of kicking the can down the road.
"The Trustees recommend that lawmakers address the projected trust fund shortfalls in a timely way in order to phase in necessary changes gradually and give workers and beneficiaries time to adjust to them," this year's report says. "Implementing changes sooner rather than later would allow more generations to share in the needed revenue increases or reductions in scheduled benefits."
Social Security's 75-year actuarial deficit is $13.9 trillion. In order for its two funds to remain solvent over that period, payroll taxes would have to be increased by 2.7 percent to 15.1 percent, or benefits would have to be reduced by 17 percent for all current and future beneficiaries, or a combination of each approach could be applied, the report says.
"If actions are deferred for several years, the changes necessary to maintain Social Security solvency become concentrated on fewer years and fewer generations," the Trustees say.
Inside the numbers
An estimated 176 million people had earnings covered by payroll and Social Security taxes in 2018. About 52.7 million people received $845 billion in retirement benefits, and 10.2 million received $143.7 billion in disability payments. Social Security is expected to pay benefits to about 64 million beneficiaries in 2019.
The OASI program took in $715.9 billion in payroll taxes, $34.5 billion in taxes on Social Security benefits, and $80.7 billion in interest payments on invested reserves.
The DI program took in $169.2 billion in payroll taxes, accounting for most of its $25.5 billion surplus in 2018.
Both programs are facing considerable demographic headwinds with the retirement of baby boomers. There were about 2.8 workers for every Social Security beneficiary in 2018.
That ratio was 3.2 to 3.4 between 1974 and 2008. It is expected to continue to decline through 2035, when it will be 2.2 workers per beneficiary, as the baby boomer generation becomes fully retired.
Social Security is about to pay out more money than it earns for the first time in decades, according to the 2019 OASDI Trustees Report, released today.
By 2020, obligations to retirees and disabled Americans will cost more than Social Security's revenue from payroll taxes, taxes on benefits, and interest earned on investments.
That imbalance is expected to continue until the SSA's main trust fund-the Old-Age and Survivors Insurance fund-is depleted in 2034, at which time scheduled benefits would be cut 23 percent to retirees. This year's projection is inline with last year's Trustees Report.
Social Security's other trust fund-the much smaller Disability Insurance Fund-is in much better shape than previously projected. The DI Fund is now projected to remain solvent to 2052, a 20-year improvement over last year's projection, owed to the continued decline of disability applications since the end of the Great Recession.
Together, OASI and DI funds will be depleted in 2035, a one-year improvement over last year's projection, the report says.
But that headline is potentially misleading. The report notes that under current law, the cuts in scheduled benefits begin separately for each program: 2034 for the OASI program, and 2052 for the DI program.
Last time SS was revenue negative, Congress moved to reform funding
When Social Security begins drawing down its $2.9 trillion in reserves next year, it will be the first time the agency will pay out more than it takes in since 1982.
That underscored the imminent funding issues Social Security was then facing, and spurred amendments that were signed into law in 1983 that included the taxation of some Social Security benefits, an increase in the retirement age, and coverage of federal employees.
Back then, control of Congress was divided as it is today-Democrats controlled the House of Representatives, Republicans controlled the Senate. The amendments were passed with bipartisan support and signed in to law by President Regan.
While Democrats and Republicans have introduced bills to reform Social Security in recent Congressional sessions, and the House Ways and Means Committee held a productive hearing on reform at the outset of the 116th Congress, the parties are at loggerheads over a path to solvency.
Democratic proposals include a phased-in increase of the payroll tax for all Americans, and an expansion of benefits for the most vulnerable Americans. Republican proposals favor raising the retirement age.
As it has in previous years, the Trustees Report urges immediate attention from lawmakers, and warns against the costs of kicking the can down the road.
"The Trustees recommend that lawmakers address the projected trust fund shortfalls in a timely way in order to phase in necessary changes gradually and give workers and beneficiaries time to adjust to them," this year's report says. "Implementing changes sooner rather than later would allow more generations to share in the needed revenue increases or reductions in scheduled benefits."
Social Security's 75-year actuarial deficit is $13.9 trillion. In order for its two funds to remain solvent over that period, payroll taxes would have to be increased by 2.7 percent to 15.1 percent, or benefits would have to be reduced by 17 percent for all current and future beneficiaries, or a combination of each approach could be applied, the report says.
"If actions are deferred for several years, the changes necessary to maintain Social Security solvency become concentrated on fewer years and fewer generations," the Trustees say.
Inside the numbers
An estimated 176 million people had earnings covered by payroll and Social Security taxes in 2018. About 52.7 million people received $845 billion in retirement benefits, and 10.2 million received $143.7 billion in disability payments. Social Security is expected to pay benefits to about 64 million beneficiaries in 2019.
The OASI program took in $715.9 billion in payroll taxes, $34.5 billion in taxes on Social Security benefits, and $80.7 billion in interest payments on invested reserves.
The DI program took in $169.2 billion in payroll taxes, accounting for most of its $25.5 billion surplus in 2018.
Both programs are facing considerable demographic headwinds with the retirement of baby boomers. There were about 2.8 workers for every Social Security beneficiary in 2018.
That ratio was 3.2 to 3.4 between 1974 and 2008. It is expected to continue to decline through 2035, when it will be 2.2 workers per beneficiary, as the baby boomer generation becomes fully retired.
Take advantage of what insurance companies have always known.
Thursday, April 4, 2019 Craig E. Chapin
 Aetna, Cigna, United Healthcare lead the change in group health insurance for small employers; however, the next step is to take advantage of how they make their profits.
Level funding is an effective first step in controlling group health premiums for small employers. However, it's essential to not overlook the basic foundation of all insurance and obtain what may be the most significant savings opportunity.
Level funded plans are considered fair insurance as they return a percentage of the premium with good claims experience but do not charge you more than the planned premium with bad claims experience. Level funded plans also bypass many of the taxes that the Affordable Care Act applies on fully insured plans. Initially, the quoted premium savings is obtained by considering the health of the participants and past medical history.
To clarify how level funding plans are designed, you must look at three premium components.
Aetna, Cigna, United Healthcare lead the change in group health insurance for small employers; however, the next step is to take advantage of how they make their profits.
Level funding is an effective first step in controlling group health premiums for small employers. However, it's essential to not overlook the basic foundation of all insurance and obtain what may be the most significant savings opportunity.
Level funded plans are considered fair insurance as they return a percentage of the premium with good claims experience but do not charge you more than the planned premium with bad claims experience. Level funded plans also bypass many of the taxes that the Affordable Care Act applies on fully insured plans. Initially, the quoted premium savings is obtained by considering the health of the participants and past medical history.
To clarify how level funding plans are designed, you must look at three premium components.
 Aetna, Cigna, United Healthcare lead the change in group health insurance for small employers; however, the next step is to take advantage of how they make their profits.
Level funding is an effective first step in controlling group health premiums for small employers. However, it's essential to not overlook the basic foundation of all insurance and obtain what may be the most significant savings opportunity.
Level funded plans are considered fair insurance as they return a percentage of the premium with good claims experience but do not charge you more than the planned premium with bad claims experience. Level funded plans also bypass many of the taxes that the Affordable Care Act applies on fully insured plans. Initially, the quoted premium savings is obtained by considering the health of the participants and past medical history.
To clarify how level funding plans are designed, you must look at three premium components.
Aetna, Cigna, United Healthcare lead the change in group health insurance for small employers; however, the next step is to take advantage of how they make their profits.
Level funding is an effective first step in controlling group health premiums for small employers. However, it's essential to not overlook the basic foundation of all insurance and obtain what may be the most significant savings opportunity.
Level funded plans are considered fair insurance as they return a percentage of the premium with good claims experience but do not charge you more than the planned premium with bad claims experience. Level funded plans also bypass many of the taxes that the Affordable Care Act applies on fully insured plans. Initially, the quoted premium savings is obtained by considering the health of the participants and past medical history.
To clarify how level funding plans are designed, you must look at three premium components.
- Stop-loss premiums protect any one person in the group or the overall group from a loss over a specific amount.
- The claims pool is roughly one-third of the overall premium and is the expected claims that are shared with the employer at the end of the year with low medical expense.
- The remaining premiums are used for administration including, network access, PBMs, claims adjudication, commissions, and support.
Let's start teaching the younger generation about fundamentals of debt.
Thursday, April 2, 2019 Craig Chapin
 Medicare for all is a dream which can never be achieved. Why talk about adding benefits when the Congressional Research Service June 2018 study projects that the trust will be insolvent by 2026? Doubling down by putting more people in the program is our politicians' way of not addressing the issue. The number one-way Medicare and Medicare save money are by paying far less than traditional insurance to doctor and hospitals. Will doctors continue to practice medicine or the pharmaceutical companies invest in R&D if they deliver services at a loss?
In 2014, there were 46.2 million Americans aged 65 and over and 6.2 million of the population aged 85 and over. The number of people aged 65 and older is expected to increase significantly and double in numbers, reaching 98.2 million by 2060. As for the number of people aged 85 and older, they are expected to triple and reach 19.7 million. How do our lawmakers plan to cover this cost before considering covering more people?
Obamacare was an entitlement expansion on Medicaid, and no one is addressing the unpaid cost of this program. The Children Health Insurance Program is the number one insurance for children aged 0 to 18, and this program will bankrupt every state if ordered to pay the entire cost. Unfortunately, our politicians continue to add entitlements and not pay for the existing programs. Our great country cannot figure out how to pay off the current $22 trillion in debt, which means the average American household carries a debt of $137,063. The U.S. Census Bureau reports the median household income was just $59,039 last year.
I won't even go near the Green initiative when the same politicians want to pass an infrastructure bill adding to the current debt. We are two interest points away from having an eye-opening situation as the debt interest payments at state and federal level will be too high to cover. Everyone needs to stop dreaming and face the facts.
Medicare for all is a dream which can never be achieved. Why talk about adding benefits when the Congressional Research Service June 2018 study projects that the trust will be insolvent by 2026? Doubling down by putting more people in the program is our politicians' way of not addressing the issue. The number one-way Medicare and Medicare save money are by paying far less than traditional insurance to doctor and hospitals. Will doctors continue to practice medicine or the pharmaceutical companies invest in R&D if they deliver services at a loss?
In 2014, there were 46.2 million Americans aged 65 and over and 6.2 million of the population aged 85 and over. The number of people aged 65 and older is expected to increase significantly and double in numbers, reaching 98.2 million by 2060. As for the number of people aged 85 and older, they are expected to triple and reach 19.7 million. How do our lawmakers plan to cover this cost before considering covering more people?
Obamacare was an entitlement expansion on Medicaid, and no one is addressing the unpaid cost of this program. The Children Health Insurance Program is the number one insurance for children aged 0 to 18, and this program will bankrupt every state if ordered to pay the entire cost. Unfortunately, our politicians continue to add entitlements and not pay for the existing programs. Our great country cannot figure out how to pay off the current $22 trillion in debt, which means the average American household carries a debt of $137,063. The U.S. Census Bureau reports the median household income was just $59,039 last year.
I won't even go near the Green initiative when the same politicians want to pass an infrastructure bill adding to the current debt. We are two interest points away from having an eye-opening situation as the debt interest payments at state and federal level will be too high to cover. Everyone needs to stop dreaming and face the facts.
 Medicare for all is a dream which can never be achieved. Why talk about adding benefits when the Congressional Research Service June 2018 study projects that the trust will be insolvent by 2026? Doubling down by putting more people in the program is our politicians' way of not addressing the issue. The number one-way Medicare and Medicare save money are by paying far less than traditional insurance to doctor and hospitals. Will doctors continue to practice medicine or the pharmaceutical companies invest in R&D if they deliver services at a loss?
In 2014, there were 46.2 million Americans aged 65 and over and 6.2 million of the population aged 85 and over. The number of people aged 65 and older is expected to increase significantly and double in numbers, reaching 98.2 million by 2060. As for the number of people aged 85 and older, they are expected to triple and reach 19.7 million. How do our lawmakers plan to cover this cost before considering covering more people?
Obamacare was an entitlement expansion on Medicaid, and no one is addressing the unpaid cost of this program. The Children Health Insurance Program is the number one insurance for children aged 0 to 18, and this program will bankrupt every state if ordered to pay the entire cost. Unfortunately, our politicians continue to add entitlements and not pay for the existing programs. Our great country cannot figure out how to pay off the current $22 trillion in debt, which means the average American household carries a debt of $137,063. The U.S. Census Bureau reports the median household income was just $59,039 last year.
I won't even go near the Green initiative when the same politicians want to pass an infrastructure bill adding to the current debt. We are two interest points away from having an eye-opening situation as the debt interest payments at state and federal level will be too high to cover. Everyone needs to stop dreaming and face the facts.
Medicare for all is a dream which can never be achieved. Why talk about adding benefits when the Congressional Research Service June 2018 study projects that the trust will be insolvent by 2026? Doubling down by putting more people in the program is our politicians' way of not addressing the issue. The number one-way Medicare and Medicare save money are by paying far less than traditional insurance to doctor and hospitals. Will doctors continue to practice medicine or the pharmaceutical companies invest in R&D if they deliver services at a loss?
In 2014, there were 46.2 million Americans aged 65 and over and 6.2 million of the population aged 85 and over. The number of people aged 65 and older is expected to increase significantly and double in numbers, reaching 98.2 million by 2060. As for the number of people aged 85 and older, they are expected to triple and reach 19.7 million. How do our lawmakers plan to cover this cost before considering covering more people?
Obamacare was an entitlement expansion on Medicaid, and no one is addressing the unpaid cost of this program. The Children Health Insurance Program is the number one insurance for children aged 0 to 18, and this program will bankrupt every state if ordered to pay the entire cost. Unfortunately, our politicians continue to add entitlements and not pay for the existing programs. Our great country cannot figure out how to pay off the current $22 trillion in debt, which means the average American household carries a debt of $137,063. The U.S. Census Bureau reports the median household income was just $59,039 last year.
I won't even go near the Green initiative when the same politicians want to pass an infrastructure bill adding to the current debt. We are two interest points away from having an eye-opening situation as the debt interest payments at state and federal level will be too high to cover. Everyone needs to stop dreaming and face the facts.
Government waste at its finest!
Friday, March 08, 2019 CEC
 In June 2018, Gov. Phil Murphy started the New Jersey state reinsurance program to stabilize the individual insurance market for 330,000 individual participants. The reinsurance program is funded by the federal and state government and reimburses insurance carriers for up to 60% of the cost of claims that fall between $40,000 and $215,000. On certain benchmark plans, participants can enjoy a reduction of about $100 a month. The governor hoped this would attract thousands of new customers to the market; however, it didn't fall up to expectations.
Roughly 255,000 individuals in NJ are covered through the federal government subsidized exchanges, which pay premiums based on income, not insurance premiums. The state's $144 million contributions would have been better spent giving the money to the 75,000 individuals currently not getting subsidies from the marketplace.
After all, dividing $144 million by 75,000 would give each person over $1,920 a year. Include the Federal contribution of $116 million to the reinsurance pool and the reduction would be $3,466.00. Even if you divide the $260 million by the 330,000 market, you will get a reduction of over $787 per person. Is this a smart use of funds?
Sources: NJ Spotlight LihoH. Stainton January 9, 2019
In June 2018, Gov. Phil Murphy started the New Jersey state reinsurance program to stabilize the individual insurance market for 330,000 individual participants. The reinsurance program is funded by the federal and state government and reimburses insurance carriers for up to 60% of the cost of claims that fall between $40,000 and $215,000. On certain benchmark plans, participants can enjoy a reduction of about $100 a month. The governor hoped this would attract thousands of new customers to the market; however, it didn't fall up to expectations.
Roughly 255,000 individuals in NJ are covered through the federal government subsidized exchanges, which pay premiums based on income, not insurance premiums. The state's $144 million contributions would have been better spent giving the money to the 75,000 individuals currently not getting subsidies from the marketplace.
After all, dividing $144 million by 75,000 would give each person over $1,920 a year. Include the Federal contribution of $116 million to the reinsurance pool and the reduction would be $3,466.00. Even if you divide the $260 million by the 330,000 market, you will get a reduction of over $787 per person. Is this a smart use of funds?
Sources: NJ Spotlight LihoH. Stainton January 9, 2019
 In June 2018, Gov. Phil Murphy started the New Jersey state reinsurance program to stabilize the individual insurance market for 330,000 individual participants. The reinsurance program is funded by the federal and state government and reimburses insurance carriers for up to 60% of the cost of claims that fall between $40,000 and $215,000. On certain benchmark plans, participants can enjoy a reduction of about $100 a month. The governor hoped this would attract thousands of new customers to the market; however, it didn't fall up to expectations.
Roughly 255,000 individuals in NJ are covered through the federal government subsidized exchanges, which pay premiums based on income, not insurance premiums. The state's $144 million contributions would have been better spent giving the money to the 75,000 individuals currently not getting subsidies from the marketplace.
After all, dividing $144 million by 75,000 would give each person over $1,920 a year. Include the Federal contribution of $116 million to the reinsurance pool and the reduction would be $3,466.00. Even if you divide the $260 million by the 330,000 market, you will get a reduction of over $787 per person. Is this a smart use of funds?
Sources: NJ Spotlight LihoH. Stainton January 9, 2019
In June 2018, Gov. Phil Murphy started the New Jersey state reinsurance program to stabilize the individual insurance market for 330,000 individual participants. The reinsurance program is funded by the federal and state government and reimburses insurance carriers for up to 60% of the cost of claims that fall between $40,000 and $215,000. On certain benchmark plans, participants can enjoy a reduction of about $100 a month. The governor hoped this would attract thousands of new customers to the market; however, it didn't fall up to expectations.
Roughly 255,000 individuals in NJ are covered through the federal government subsidized exchanges, which pay premiums based on income, not insurance premiums. The state's $144 million contributions would have been better spent giving the money to the 75,000 individuals currently not getting subsidies from the marketplace.
After all, dividing $144 million by 75,000 would give each person over $1,920 a year. Include the Federal contribution of $116 million to the reinsurance pool and the reduction would be $3,466.00. Even if you divide the $260 million by the 330,000 market, you will get a reduction of over $787 per person. Is this a smart use of funds?
Sources: NJ Spotlight LihoH. Stainton January 9, 2019
CHIP "Children Health Insurance Program"
Wednesday, March 06, 2019 CEC
 Data from 2014 indicates that an estimated 91% of eligible children in the United States are enrolled in Medicaid/CHIP programs. These are the children who don't have any other coverage and are fairly represented by these figures. The percentage for participants in PA was 91.90% and 93.70% in NJ. The figure is the estimated Medicaid/Children's Health Insurance Program (CHIP) participation rates for children aged 0 to 18.
Children's Health Insurance Program (CHIP) is funded jointly by the state and the federal government. In most states, the government marketplace directs all children under 19 for households earning less than 350% of the federal poverty to be enrolled in the program. Children in a family of four earning less than $88,000 are directed to Medicaid. Is this teaching our children that the government should pay for their health insurance?
On January 22, 2018, Congress passed a six-year extension of CHIP funding to provide stable funding for states to continue the program's coverage. The law continues the 23% CHIP enhanced federal match rate established by the Affordable Care Act for FY 2018 and FY 2019. The regular CHIP match rate will be implemented for FY 2021 and FY 2023. However, plans for FY 2020 show a steady decrease to 11.5%.
Currently, New Jersey Family Care covers over 1,715,602 people and represents 19.30% of the NJ population. This program also includes 51.9% of the long term care population in Home and Community-based services, including over 800,000 NJ children. On average, the federal government's share of Medicaid spending is 57%, but it is 70% under CHIP. All states know that government support is essential to sustain the program since states are incapable of continuing them on their own. The government is largely funding this program by adding to the debt. In general, Obamacare is an unfunded entitlement hidden with the excuse that pre-existing conditions would not be covered without it.
Source: https://www.insurekidsnow.gov http://www.njfamilycare.org
Data from 2014 indicates that an estimated 91% of eligible children in the United States are enrolled in Medicaid/CHIP programs. These are the children who don't have any other coverage and are fairly represented by these figures. The percentage for participants in PA was 91.90% and 93.70% in NJ. The figure is the estimated Medicaid/Children's Health Insurance Program (CHIP) participation rates for children aged 0 to 18.
Children's Health Insurance Program (CHIP) is funded jointly by the state and the federal government. In most states, the government marketplace directs all children under 19 for households earning less than 350% of the federal poverty to be enrolled in the program. Children in a family of four earning less than $88,000 are directed to Medicaid. Is this teaching our children that the government should pay for their health insurance?
On January 22, 2018, Congress passed a six-year extension of CHIP funding to provide stable funding for states to continue the program's coverage. The law continues the 23% CHIP enhanced federal match rate established by the Affordable Care Act for FY 2018 and FY 2019. The regular CHIP match rate will be implemented for FY 2021 and FY 2023. However, plans for FY 2020 show a steady decrease to 11.5%.
Currently, New Jersey Family Care covers over 1,715,602 people and represents 19.30% of the NJ population. This program also includes 51.9% of the long term care population in Home and Community-based services, including over 800,000 NJ children. On average, the federal government's share of Medicaid spending is 57%, but it is 70% under CHIP. All states know that government support is essential to sustain the program since states are incapable of continuing them on their own. The government is largely funding this program by adding to the debt. In general, Obamacare is an unfunded entitlement hidden with the excuse that pre-existing conditions would not be covered without it.
Source: https://www.insurekidsnow.gov http://www.njfamilycare.org
 Data from 2014 indicates that an estimated 91% of eligible children in the United States are enrolled in Medicaid/CHIP programs. These are the children who don't have any other coverage and are fairly represented by these figures. The percentage for participants in PA was 91.90% and 93.70% in NJ. The figure is the estimated Medicaid/Children's Health Insurance Program (CHIP) participation rates for children aged 0 to 18.
Children's Health Insurance Program (CHIP) is funded jointly by the state and the federal government. In most states, the government marketplace directs all children under 19 for households earning less than 350% of the federal poverty to be enrolled in the program. Children in a family of four earning less than $88,000 are directed to Medicaid. Is this teaching our children that the government should pay for their health insurance?
On January 22, 2018, Congress passed a six-year extension of CHIP funding to provide stable funding for states to continue the program's coverage. The law continues the 23% CHIP enhanced federal match rate established by the Affordable Care Act for FY 2018 and FY 2019. The regular CHIP match rate will be implemented for FY 2021 and FY 2023. However, plans for FY 2020 show a steady decrease to 11.5%.
Currently, New Jersey Family Care covers over 1,715,602 people and represents 19.30% of the NJ population. This program also includes 51.9% of the long term care population in Home and Community-based services, including over 800,000 NJ children. On average, the federal government's share of Medicaid spending is 57%, but it is 70% under CHIP. All states know that government support is essential to sustain the program since states are incapable of continuing them on their own. The government is largely funding this program by adding to the debt. In general, Obamacare is an unfunded entitlement hidden with the excuse that pre-existing conditions would not be covered without it.
Source: https://www.insurekidsnow.gov http://www.njfamilycare.org
Data from 2014 indicates that an estimated 91% of eligible children in the United States are enrolled in Medicaid/CHIP programs. These are the children who don't have any other coverage and are fairly represented by these figures. The percentage for participants in PA was 91.90% and 93.70% in NJ. The figure is the estimated Medicaid/Children's Health Insurance Program (CHIP) participation rates for children aged 0 to 18.
Children's Health Insurance Program (CHIP) is funded jointly by the state and the federal government. In most states, the government marketplace directs all children under 19 for households earning less than 350% of the federal poverty to be enrolled in the program. Children in a family of four earning less than $88,000 are directed to Medicaid. Is this teaching our children that the government should pay for their health insurance?
On January 22, 2018, Congress passed a six-year extension of CHIP funding to provide stable funding for states to continue the program's coverage. The law continues the 23% CHIP enhanced federal match rate established by the Affordable Care Act for FY 2018 and FY 2019. The regular CHIP match rate will be implemented for FY 2021 and FY 2023. However, plans for FY 2020 show a steady decrease to 11.5%.
Currently, New Jersey Family Care covers over 1,715,602 people and represents 19.30% of the NJ population. This program also includes 51.9% of the long term care population in Home and Community-based services, including over 800,000 NJ children. On average, the federal government's share of Medicaid spending is 57%, but it is 70% under CHIP. All states know that government support is essential to sustain the program since states are incapable of continuing them on their own. The government is largely funding this program by adding to the debt. In general, Obamacare is an unfunded entitlement hidden with the excuse that pre-existing conditions would not be covered without it.
Source: https://www.insurekidsnow.gov http://www.njfamilycare.org
A new law on Surprise Billing in NJ
Monday, July 23, 2018 by Dan Roslokken -- General counsel to Insurance Design Administrators in Oakland. He is admitted to the N.J., Pa. and U.S. Supreme Court Bars.
 On June 1, Assembly Bill 2039 became law, ushering in bold patient protections and blockbuster realignment of claims-handling processes. Effective Aug. 30, extinction of "surprise" out-of-network claims is its goal. Patient protections now secured, the true "surprise" awaits providers and carriers scrambling to meet disclosure requirements and the uncertain fiscal impact upon plans who must comply.
A New Claims Order
Protection under the act hinges upon two classifications of medical charges.
The first category addresses out-of-network services that are "knowingly, voluntarily and specifically" selected. In these circumstances, aside from brief disclosure obligations of the provider (discussed later), no further protections apply.
The second category really shakes things up. Major patient protection provisions are created. Claims practices between providers and payers are significantly modified. Namely, if services are either out-of-network "inadvertently" or are "emergent," the provider is barred from billing the patient in excess of their deductible, copayment or coinsurance obligation. This is the hallmark achievement of the act, sparing patients from so called "surprise medical billing."
This shifts the fiscal dispute. Now solely between payer and provider, the act requires plans to provide a "clear and understandable description" of their methodology to determine the allowed amount for out-of-network services. Payment is to follow. Assignment of payment to the provider is automatic under the act. If the provider disagrees with the payment, a novel and fast-tracked process awaits with arbitration at the end.
Payment and appeal is abbreviated under the act. Within 20 days of receipt, the claim is to be paid or notice provided stating the charges are considered excessive. A 30-day settlement period follows. If agreement is not reached, the payor nevertheless is to pay their "final offer." If the provider remains unsatisfied and the difference between "final offers" is greater than $1000, the provider holds a 30-day option to initiate binding arbitration through NJDOBI.
Arbitration is upon written submissions including each party's "final offer." Oddly, the act freezes the payer's position, with no ability to submit a modified "final offer." Decision is swift (within 30 days) and limited to the two amounts submitted. No discretion exists to fashion a different amount (having been deleted in the final version of the bill). Fees and costs are split, unless the arbitrator finds the payor failed to act in good faith. No mirror provision exists for providers failing to act in good faith. Payment (if any), is to be made within 20 days of decision. Interest rates apply thereafter.
Arbitration is barred for those not following pre-authorization or medical necessity review requirements. Similarly, arbitration is unavailable for those who have knowingly and voluntarily selected out-of-network services.
"Inadvertent" ... or by Design?
Importance hinges upon whether services were "inadvertently" out of network, defined as "[when] for any reason in-network services are unavailable in that facility." The phrasing is significant. Common hospital practice outsources departments, frequently including emergency rooms, radiology, lab services and anesthesiology-such services seldom participating with any carrier. It is precisely this mismatch of participation status that leads to the so-called surprise bills.
But rather than tackle root causes, the act goes in a different direction, calling it inadvertent when participating services are "unavailable" "for any reason" (arguably including having outsourced the services in the first place). The result deems all such services as "inadvertent," enjoying the protections of fast track payment and arbitration. The underlying practice is unaddressed and, by virtue of this act, is now protected.
All Is Not Roses for Facilities
It is not all upside. The act requires facilities to advise patients of their participating status, directing patients to also confirm the participation status of the provider arranging the service(s). Differences in disclosure depend upon the participation status of the facility. A significant twist lies in defining "facility" beyond the traditional concept of a hospital to include broader categories of satellite emergency departments, hospital-based off-site ambulatory care facilities, and free-standing ambulatory surgical centers.
The act also requires facility website-based disclosure covering four topics: plans in which the facility participates; notice that physician services are not included in the facility charges; full contact information for all hospital-based groups contracted by the facility (to include anesthesiology, pathology and radiology); and finally, the full contact information of every physician employed at the facility and the plans in which they participate. Disclosure forms will be regulated by the Department of Health.
Tougher Disclosure for Providers
The burden of disclosure (and modified billing practices) falls even harder upon providers.
Either via website or written notice, providers are to list the plans in which they participate. Where the provider does not participate in a plan, the provider is to inform the patient in terms "typically understood" of their non-participating status, and their charges must be available upon request. If requested, the provider is to provide the procedure codes anticipated for the service(s) and their charges. Further, notice is to be given that the patient may be responsible for amounts in excess of the person's deductible, coinsurance and copayment for any out-of-network services and to contact their carrier for further information.
Referrals and coordinated treatment bring additional responsibilities. Regardless of setting, the originating provider is to disclose the full contact information of any provider scheduled to provide anesthesiology, laboratory, pathology, radiology or assistant surgery services, advising the patient to determine the plan participation status of referred providers. Disclosure expands when scheduled facility and non-facility services are involved to include the full contact information of any other physician whose services are scheduled at the time of pre-admission testing, registration or admission. Licensing boards are delegated oversight of disclosure forms and sufficiency.
Boldly, the act modifies billing practices associated with the waiving of patient responsibilities. A hotly debated practice, the act now forbids providers from waiving any part of a deductible, copayment or coinsurance "as an inducement" to entice patients to utilize their out-of-network services. If a pattern of such waiver is established, the "inducement" is considered satisfied (and a violative practice).
Carrier Lift
The toughest responsibilities are placed upon carriers. Beyond listing providers who participate with the carrier, the methodology that determines the allowed amount for out-of-network services is to be disclosed. Moreover, carriers are to enable a website to not only calculate reimbursement rates for out-of-network services, but their difference from the usual and customary cost. Now obliged to staff customer service hotlines 16 hours per day, the carrier is responsible to state the allowed amount the plan will reimburse for a particular medical procedure (CPT code) and the portion of the allowed amount for which the patient will be responsible.
Carriers are to alter their Explanation of Benefits to clearly state the protections against balance billing for inadvertent and emergent services. NJDOBI is directed to design new medical identification cards consistent with the protections under the act. Tabulations of realized savings under the act are to be filed annually with NJDOBI.
Broad brushed, annual independent third-party audits of any "managed care plan" are mandated under the act. While the scope is unclear, apparently audits are to opine upon the adequacy of providers "in accordance with applicable federal or state law." Results will be posted on NJDOBI's website and deficiencies can trigger NJDOBI enforcement.
Self-Funded Plans and the Illusion of Opting In
Recognizing that not all plans are fully insured with a carrier, the act acknowledges that health benefits can be self-funded. Numerous references are made to self-funded plans' ability to opt in to the act's new world order of claims resolution. Whether plans do so is irrelevant, as the act permits providers to initiate arbitration upon all self-funded plans without qualification. The only difference for a non-opting-in self-funded plan is the decision maker's discretion to fashion an award (the concept of either/or and "final offers" does not apply). Whether arbitration is binding is unclear, the act conflictingly stating both.
Further inartful phrasing limits self-funded plans to those regulated under ERISA. This leaves the status unclear for a substantial subset of plans neither fully insured nor self-insured under ERISA-e.g. MEWAs (multiple employer welfare arrangements), association plans and church plans-in addition to government entities permitted to self fund, which includes the NJ State Health Benefit Program, HIFs, counties, municipalities and agencies.
Only the Beginning?
Patient protection is always the goal. But it did not have to be this way. Or so complicated.
Inclusion of the Medicare Allowable Charge upon all billing (a current federal proposal) would have benchmarked the relative value the act clumsily mishandles. The existing statute regarding excessive fees could have been modified to declare charges in excess of "x" times the Medicare Allowable Charge to be de facto excessive and barred. Alternatively, a requirement could have been made that all contracted services to hospitals and all employee physicians of a hospital mirror its participation status.
Instead, the act is hastily written, contradicting itself at times, ignoring existing state and federal claims handling and appeal rights. Conflict of laws and federal pre-emption challenges will plague implementation. The data lift of carriers and providers is substantial. The authority in arbitration to exceed stated out-of-network plan limits is unknown, but doubtful. The significance of "plans" not being synonymous with "carriers" is completely missed. Whether estimation of costs will operate as a medical version of a mechanic's pre-estimate is unsettled. Claims negotiation services are constrained due to the new processing deadlines. Because such cost saving mechanisms are curtailed, self-funded plans may be disproportionately affected, particularly those sponsored by municipalities, counties and unions.
It did not have to be this way. Or so complicated.
On June 1, Assembly Bill 2039 became law, ushering in bold patient protections and blockbuster realignment of claims-handling processes. Effective Aug. 30, extinction of "surprise" out-of-network claims is its goal. Patient protections now secured, the true "surprise" awaits providers and carriers scrambling to meet disclosure requirements and the uncertain fiscal impact upon plans who must comply.
A New Claims Order
Protection under the act hinges upon two classifications of medical charges.
The first category addresses out-of-network services that are "knowingly, voluntarily and specifically" selected. In these circumstances, aside from brief disclosure obligations of the provider (discussed later), no further protections apply.
The second category really shakes things up. Major patient protection provisions are created. Claims practices between providers and payers are significantly modified. Namely, if services are either out-of-network "inadvertently" or are "emergent," the provider is barred from billing the patient in excess of their deductible, copayment or coinsurance obligation. This is the hallmark achievement of the act, sparing patients from so called "surprise medical billing."
This shifts the fiscal dispute. Now solely between payer and provider, the act requires plans to provide a "clear and understandable description" of their methodology to determine the allowed amount for out-of-network services. Payment is to follow. Assignment of payment to the provider is automatic under the act. If the provider disagrees with the payment, a novel and fast-tracked process awaits with arbitration at the end.
Payment and appeal is abbreviated under the act. Within 20 days of receipt, the claim is to be paid or notice provided stating the charges are considered excessive. A 30-day settlement period follows. If agreement is not reached, the payor nevertheless is to pay their "final offer." If the provider remains unsatisfied and the difference between "final offers" is greater than $1000, the provider holds a 30-day option to initiate binding arbitration through NJDOBI.
Arbitration is upon written submissions including each party's "final offer." Oddly, the act freezes the payer's position, with no ability to submit a modified "final offer." Decision is swift (within 30 days) and limited to the two amounts submitted. No discretion exists to fashion a different amount (having been deleted in the final version of the bill). Fees and costs are split, unless the arbitrator finds the payor failed to act in good faith. No mirror provision exists for providers failing to act in good faith. Payment (if any), is to be made within 20 days of decision. Interest rates apply thereafter.
Arbitration is barred for those not following pre-authorization or medical necessity review requirements. Similarly, arbitration is unavailable for those who have knowingly and voluntarily selected out-of-network services.
"Inadvertent" ... or by Design?
Importance hinges upon whether services were "inadvertently" out of network, defined as "[when] for any reason in-network services are unavailable in that facility." The phrasing is significant. Common hospital practice outsources departments, frequently including emergency rooms, radiology, lab services and anesthesiology-such services seldom participating with any carrier. It is precisely this mismatch of participation status that leads to the so-called surprise bills.
But rather than tackle root causes, the act goes in a different direction, calling it inadvertent when participating services are "unavailable" "for any reason" (arguably including having outsourced the services in the first place). The result deems all such services as "inadvertent," enjoying the protections of fast track payment and arbitration. The underlying practice is unaddressed and, by virtue of this act, is now protected.
All Is Not Roses for Facilities
It is not all upside. The act requires facilities to advise patients of their participating status, directing patients to also confirm the participation status of the provider arranging the service(s). Differences in disclosure depend upon the participation status of the facility. A significant twist lies in defining "facility" beyond the traditional concept of a hospital to include broader categories of satellite emergency departments, hospital-based off-site ambulatory care facilities, and free-standing ambulatory surgical centers.
The act also requires facility website-based disclosure covering four topics: plans in which the facility participates; notice that physician services are not included in the facility charges; full contact information for all hospital-based groups contracted by the facility (to include anesthesiology, pathology and radiology); and finally, the full contact information of every physician employed at the facility and the plans in which they participate. Disclosure forms will be regulated by the Department of Health.
Tougher Disclosure for Providers
The burden of disclosure (and modified billing practices) falls even harder upon providers.
Either via website or written notice, providers are to list the plans in which they participate. Where the provider does not participate in a plan, the provider is to inform the patient in terms "typically understood" of their non-participating status, and their charges must be available upon request. If requested, the provider is to provide the procedure codes anticipated for the service(s) and their charges. Further, notice is to be given that the patient may be responsible for amounts in excess of the person's deductible, coinsurance and copayment for any out-of-network services and to contact their carrier for further information.
Referrals and coordinated treatment bring additional responsibilities. Regardless of setting, the originating provider is to disclose the full contact information of any provider scheduled to provide anesthesiology, laboratory, pathology, radiology or assistant surgery services, advising the patient to determine the plan participation status of referred providers. Disclosure expands when scheduled facility and non-facility services are involved to include the full contact information of any other physician whose services are scheduled at the time of pre-admission testing, registration or admission. Licensing boards are delegated oversight of disclosure forms and sufficiency.
Boldly, the act modifies billing practices associated with the waiving of patient responsibilities. A hotly debated practice, the act now forbids providers from waiving any part of a deductible, copayment or coinsurance "as an inducement" to entice patients to utilize their out-of-network services. If a pattern of such waiver is established, the "inducement" is considered satisfied (and a violative practice).
Carrier Lift
The toughest responsibilities are placed upon carriers. Beyond listing providers who participate with the carrier, the methodology that determines the allowed amount for out-of-network services is to be disclosed. Moreover, carriers are to enable a website to not only calculate reimbursement rates for out-of-network services, but their difference from the usual and customary cost. Now obliged to staff customer service hotlines 16 hours per day, the carrier is responsible to state the allowed amount the plan will reimburse for a particular medical procedure (CPT code) and the portion of the allowed amount for which the patient will be responsible.
Carriers are to alter their Explanation of Benefits to clearly state the protections against balance billing for inadvertent and emergent services. NJDOBI is directed to design new medical identification cards consistent with the protections under the act. Tabulations of realized savings under the act are to be filed annually with NJDOBI.
Broad brushed, annual independent third-party audits of any "managed care plan" are mandated under the act. While the scope is unclear, apparently audits are to opine upon the adequacy of providers "in accordance with applicable federal or state law." Results will be posted on NJDOBI's website and deficiencies can trigger NJDOBI enforcement.
Self-Funded Plans and the Illusion of Opting In
Recognizing that not all plans are fully insured with a carrier, the act acknowledges that health benefits can be self-funded. Numerous references are made to self-funded plans' ability to opt in to the act's new world order of claims resolution. Whether plans do so is irrelevant, as the act permits providers to initiate arbitration upon all self-funded plans without qualification. The only difference for a non-opting-in self-funded plan is the decision maker's discretion to fashion an award (the concept of either/or and "final offers" does not apply). Whether arbitration is binding is unclear, the act conflictingly stating both.
Further inartful phrasing limits self-funded plans to those regulated under ERISA. This leaves the status unclear for a substantial subset of plans neither fully insured nor self-insured under ERISA-e.g. MEWAs (multiple employer welfare arrangements), association plans and church plans-in addition to government entities permitted to self fund, which includes the NJ State Health Benefit Program, HIFs, counties, municipalities and agencies.
Only the Beginning?
Patient protection is always the goal. But it did not have to be this way. Or so complicated.
Inclusion of the Medicare Allowable Charge upon all billing (a current federal proposal) would have benchmarked the relative value the act clumsily mishandles. The existing statute regarding excessive fees could have been modified to declare charges in excess of "x" times the Medicare Allowable Charge to be de facto excessive and barred. Alternatively, a requirement could have been made that all contracted services to hospitals and all employee physicians of a hospital mirror its participation status.
Instead, the act is hastily written, contradicting itself at times, ignoring existing state and federal claims handling and appeal rights. Conflict of laws and federal pre-emption challenges will plague implementation. The data lift of carriers and providers is substantial. The authority in arbitration to exceed stated out-of-network plan limits is unknown, but doubtful. The significance of "plans" not being synonymous with "carriers" is completely missed. Whether estimation of costs will operate as a medical version of a mechanic's pre-estimate is unsettled. Claims negotiation services are constrained due to the new processing deadlines. Because such cost saving mechanisms are curtailed, self-funded plans may be disproportionately affected, particularly those sponsored by municipalities, counties and unions.
It did not have to be this way. Or so complicated.
 On June 1, Assembly Bill 2039 became law, ushering in bold patient protections and blockbuster realignment of claims-handling processes. Effective Aug. 30, extinction of "surprise" out-of-network claims is its goal. Patient protections now secured, the true "surprise" awaits providers and carriers scrambling to meet disclosure requirements and the uncertain fiscal impact upon plans who must comply.
A New Claims Order
Protection under the act hinges upon two classifications of medical charges.
The first category addresses out-of-network services that are "knowingly, voluntarily and specifically" selected. In these circumstances, aside from brief disclosure obligations of the provider (discussed later), no further protections apply.
The second category really shakes things up. Major patient protection provisions are created. Claims practices between providers and payers are significantly modified. Namely, if services are either out-of-network "inadvertently" or are "emergent," the provider is barred from billing the patient in excess of their deductible, copayment or coinsurance obligation. This is the hallmark achievement of the act, sparing patients from so called "surprise medical billing."
This shifts the fiscal dispute. Now solely between payer and provider, the act requires plans to provide a "clear and understandable description" of their methodology to determine the allowed amount for out-of-network services. Payment is to follow. Assignment of payment to the provider is automatic under the act. If the provider disagrees with the payment, a novel and fast-tracked process awaits with arbitration at the end.
Payment and appeal is abbreviated under the act. Within 20 days of receipt, the claim is to be paid or notice provided stating the charges are considered excessive. A 30-day settlement period follows. If agreement is not reached, the payor nevertheless is to pay their "final offer." If the provider remains unsatisfied and the difference between "final offers" is greater than $1000, the provider holds a 30-day option to initiate binding arbitration through NJDOBI.
Arbitration is upon written submissions including each party's "final offer." Oddly, the act freezes the payer's position, with no ability to submit a modified "final offer." Decision is swift (within 30 days) and limited to the two amounts submitted. No discretion exists to fashion a different amount (having been deleted in the final version of the bill). Fees and costs are split, unless the arbitrator finds the payor failed to act in good faith. No mirror provision exists for providers failing to act in good faith. Payment (if any), is to be made within 20 days of decision. Interest rates apply thereafter.
Arbitration is barred for those not following pre-authorization or medical necessity review requirements. Similarly, arbitration is unavailable for those who have knowingly and voluntarily selected out-of-network services.
"Inadvertent" ... or by Design?
Importance hinges upon whether services were "inadvertently" out of network, defined as "[when] for any reason in-network services are unavailable in that facility." The phrasing is significant. Common hospital practice outsources departments, frequently including emergency rooms, radiology, lab services and anesthesiology-such services seldom participating with any carrier. It is precisely this mismatch of participation status that leads to the so-called surprise bills.
But rather than tackle root causes, the act goes in a different direction, calling it inadvertent when participating services are "unavailable" "for any reason" (arguably including having outsourced the services in the first place). The result deems all such services as "inadvertent," enjoying the protections of fast track payment and arbitration. The underlying practice is unaddressed and, by virtue of this act, is now protected.
All Is Not Roses for Facilities
It is not all upside. The act requires facilities to advise patients of their participating status, directing patients to also confirm the participation status of the provider arranging the service(s). Differences in disclosure depend upon the participation status of the facility. A significant twist lies in defining "facility" beyond the traditional concept of a hospital to include broader categories of satellite emergency departments, hospital-based off-site ambulatory care facilities, and free-standing ambulatory surgical centers.
The act also requires facility website-based disclosure covering four topics: plans in which the facility participates; notice that physician services are not included in the facility charges; full contact information for all hospital-based groups contracted by the facility (to include anesthesiology, pathology and radiology); and finally, the full contact information of every physician employed at the facility and the plans in which they participate. Disclosure forms will be regulated by the Department of Health.
Tougher Disclosure for Providers
The burden of disclosure (and modified billing practices) falls even harder upon providers.
Either via website or written notice, providers are to list the plans in which they participate. Where the provider does not participate in a plan, the provider is to inform the patient in terms "typically understood" of their non-participating status, and their charges must be available upon request. If requested, the provider is to provide the procedure codes anticipated for the service(s) and their charges. Further, notice is to be given that the patient may be responsible for amounts in excess of the person's deductible, coinsurance and copayment for any out-of-network services and to contact their carrier for further information.
Referrals and coordinated treatment bring additional responsibilities. Regardless of setting, the originating provider is to disclose the full contact information of any provider scheduled to provide anesthesiology, laboratory, pathology, radiology or assistant surgery services, advising the patient to determine the plan participation status of referred providers. Disclosure expands when scheduled facility and non-facility services are involved to include the full contact information of any other physician whose services are scheduled at the time of pre-admission testing, registration or admission. Licensing boards are delegated oversight of disclosure forms and sufficiency.
Boldly, the act modifies billing practices associated with the waiving of patient responsibilities. A hotly debated practice, the act now forbids providers from waiving any part of a deductible, copayment or coinsurance "as an inducement" to entice patients to utilize their out-of-network services. If a pattern of such waiver is established, the "inducement" is considered satisfied (and a violative practice).
Carrier Lift
The toughest responsibilities are placed upon carriers. Beyond listing providers who participate with the carrier, the methodology that determines the allowed amount for out-of-network services is to be disclosed. Moreover, carriers are to enable a website to not only calculate reimbursement rates for out-of-network services, but their difference from the usual and customary cost. Now obliged to staff customer service hotlines 16 hours per day, the carrier is responsible to state the allowed amount the plan will reimburse for a particular medical procedure (CPT code) and the portion of the allowed amount for which the patient will be responsible.
Carriers are to alter their Explanation of Benefits to clearly state the protections against balance billing for inadvertent and emergent services. NJDOBI is directed to design new medical identification cards consistent with the protections under the act. Tabulations of realized savings under the act are to be filed annually with NJDOBI.
Broad brushed, annual independent third-party audits of any "managed care plan" are mandated under the act. While the scope is unclear, apparently audits are to opine upon the adequacy of providers "in accordance with applicable federal or state law." Results will be posted on NJDOBI's website and deficiencies can trigger NJDOBI enforcement.
Self-Funded Plans and the Illusion of Opting In
Recognizing that not all plans are fully insured with a carrier, the act acknowledges that health benefits can be self-funded. Numerous references are made to self-funded plans' ability to opt in to the act's new world order of claims resolution. Whether plans do so is irrelevant, as the act permits providers to initiate arbitration upon all self-funded plans without qualification. The only difference for a non-opting-in self-funded plan is the decision maker's discretion to fashion an award (the concept of either/or and "final offers" does not apply). Whether arbitration is binding is unclear, the act conflictingly stating both.
Further inartful phrasing limits self-funded plans to those regulated under ERISA. This leaves the status unclear for a substantial subset of plans neither fully insured nor self-insured under ERISA-e.g. MEWAs (multiple employer welfare arrangements), association plans and church plans-in addition to government entities permitted to self fund, which includes the NJ State Health Benefit Program, HIFs, counties, municipalities and agencies.
Only the Beginning?
Patient protection is always the goal. But it did not have to be this way. Or so complicated.
Inclusion of the Medicare Allowable Charge upon all billing (a current federal proposal) would have benchmarked the relative value the act clumsily mishandles. The existing statute regarding excessive fees could have been modified to declare charges in excess of "x" times the Medicare Allowable Charge to be de facto excessive and barred. Alternatively, a requirement could have been made that all contracted services to hospitals and all employee physicians of a hospital mirror its participation status.
Instead, the act is hastily written, contradicting itself at times, ignoring existing state and federal claims handling and appeal rights. Conflict of laws and federal pre-emption challenges will plague implementation. The data lift of carriers and providers is substantial. The authority in arbitration to exceed stated out-of-network plan limits is unknown, but doubtful. The significance of "plans" not being synonymous with "carriers" is completely missed. Whether estimation of costs will operate as a medical version of a mechanic's pre-estimate is unsettled. Claims negotiation services are constrained due to the new processing deadlines. Because such cost saving mechanisms are curtailed, self-funded plans may be disproportionately affected, particularly those sponsored by municipalities, counties and unions.
It did not have to be this way. Or so complicated.
On June 1, Assembly Bill 2039 became law, ushering in bold patient protections and blockbuster realignment of claims-handling processes. Effective Aug. 30, extinction of "surprise" out-of-network claims is its goal. Patient protections now secured, the true "surprise" awaits providers and carriers scrambling to meet disclosure requirements and the uncertain fiscal impact upon plans who must comply.
A New Claims Order
Protection under the act hinges upon two classifications of medical charges.
The first category addresses out-of-network services that are "knowingly, voluntarily and specifically" selected. In these circumstances, aside from brief disclosure obligations of the provider (discussed later), no further protections apply.
The second category really shakes things up. Major patient protection provisions are created. Claims practices between providers and payers are significantly modified. Namely, if services are either out-of-network "inadvertently" or are "emergent," the provider is barred from billing the patient in excess of their deductible, copayment or coinsurance obligation. This is the hallmark achievement of the act, sparing patients from so called "surprise medical billing."
This shifts the fiscal dispute. Now solely between payer and provider, the act requires plans to provide a "clear and understandable description" of their methodology to determine the allowed amount for out-of-network services. Payment is to follow. Assignment of payment to the provider is automatic under the act. If the provider disagrees with the payment, a novel and fast-tracked process awaits with arbitration at the end.
Payment and appeal is abbreviated under the act. Within 20 days of receipt, the claim is to be paid or notice provided stating the charges are considered excessive. A 30-day settlement period follows. If agreement is not reached, the payor nevertheless is to pay their "final offer." If the provider remains unsatisfied and the difference between "final offers" is greater than $1000, the provider holds a 30-day option to initiate binding arbitration through NJDOBI.
Arbitration is upon written submissions including each party's "final offer." Oddly, the act freezes the payer's position, with no ability to submit a modified "final offer." Decision is swift (within 30 days) and limited to the two amounts submitted. No discretion exists to fashion a different amount (having been deleted in the final version of the bill). Fees and costs are split, unless the arbitrator finds the payor failed to act in good faith. No mirror provision exists for providers failing to act in good faith. Payment (if any), is to be made within 20 days of decision. Interest rates apply thereafter.
Arbitration is barred for those not following pre-authorization or medical necessity review requirements. Similarly, arbitration is unavailable for those who have knowingly and voluntarily selected out-of-network services.
"Inadvertent" ... or by Design?
Importance hinges upon whether services were "inadvertently" out of network, defined as "[when] for any reason in-network services are unavailable in that facility." The phrasing is significant. Common hospital practice outsources departments, frequently including emergency rooms, radiology, lab services and anesthesiology-such services seldom participating with any carrier. It is precisely this mismatch of participation status that leads to the so-called surprise bills.
But rather than tackle root causes, the act goes in a different direction, calling it inadvertent when participating services are "unavailable" "for any reason" (arguably including having outsourced the services in the first place). The result deems all such services as "inadvertent," enjoying the protections of fast track payment and arbitration. The underlying practice is unaddressed and, by virtue of this act, is now protected.
All Is Not Roses for Facilities
It is not all upside. The act requires facilities to advise patients of their participating status, directing patients to also confirm the participation status of the provider arranging the service(s). Differences in disclosure depend upon the participation status of the facility. A significant twist lies in defining "facility" beyond the traditional concept of a hospital to include broader categories of satellite emergency departments, hospital-based off-site ambulatory care facilities, and free-standing ambulatory surgical centers.
The act also requires facility website-based disclosure covering four topics: plans in which the facility participates; notice that physician services are not included in the facility charges; full contact information for all hospital-based groups contracted by the facility (to include anesthesiology, pathology and radiology); and finally, the full contact information of every physician employed at the facility and the plans in which they participate. Disclosure forms will be regulated by the Department of Health.
Tougher Disclosure for Providers
The burden of disclosure (and modified billing practices) falls even harder upon providers.
Either via website or written notice, providers are to list the plans in which they participate. Where the provider does not participate in a plan, the provider is to inform the patient in terms "typically understood" of their non-participating status, and their charges must be available upon request. If requested, the provider is to provide the procedure codes anticipated for the service(s) and their charges. Further, notice is to be given that the patient may be responsible for amounts in excess of the person's deductible, coinsurance and copayment for any out-of-network services and to contact their carrier for further information.
Referrals and coordinated treatment bring additional responsibilities. Regardless of setting, the originating provider is to disclose the full contact information of any provider scheduled to provide anesthesiology, laboratory, pathology, radiology or assistant surgery services, advising the patient to determine the plan participation status of referred providers. Disclosure expands when scheduled facility and non-facility services are involved to include the full contact information of any other physician whose services are scheduled at the time of pre-admission testing, registration or admission. Licensing boards are delegated oversight of disclosure forms and sufficiency.
Boldly, the act modifies billing practices associated with the waiving of patient responsibilities. A hotly debated practice, the act now forbids providers from waiving any part of a deductible, copayment or coinsurance "as an inducement" to entice patients to utilize their out-of-network services. If a pattern of such waiver is established, the "inducement" is considered satisfied (and a violative practice).
Carrier Lift
The toughest responsibilities are placed upon carriers. Beyond listing providers who participate with the carrier, the methodology that determines the allowed amount for out-of-network services is to be disclosed. Moreover, carriers are to enable a website to not only calculate reimbursement rates for out-of-network services, but their difference from the usual and customary cost. Now obliged to staff customer service hotlines 16 hours per day, the carrier is responsible to state the allowed amount the plan will reimburse for a particular medical procedure (CPT code) and the portion of the allowed amount for which the patient will be responsible.
Carriers are to alter their Explanation of Benefits to clearly state the protections against balance billing for inadvertent and emergent services. NJDOBI is directed to design new medical identification cards consistent with the protections under the act. Tabulations of realized savings under the act are to be filed annually with NJDOBI.
Broad brushed, annual independent third-party audits of any "managed care plan" are mandated under the act. While the scope is unclear, apparently audits are to opine upon the adequacy of providers "in accordance with applicable federal or state law." Results will be posted on NJDOBI's website and deficiencies can trigger NJDOBI enforcement.
Self-Funded Plans and the Illusion of Opting In
Recognizing that not all plans are fully insured with a carrier, the act acknowledges that health benefits can be self-funded. Numerous references are made to self-funded plans' ability to opt in to the act's new world order of claims resolution. Whether plans do so is irrelevant, as the act permits providers to initiate arbitration upon all self-funded plans without qualification. The only difference for a non-opting-in self-funded plan is the decision maker's discretion to fashion an award (the concept of either/or and "final offers" does not apply). Whether arbitration is binding is unclear, the act conflictingly stating both.
Further inartful phrasing limits self-funded plans to those regulated under ERISA. This leaves the status unclear for a substantial subset of plans neither fully insured nor self-insured under ERISA-e.g. MEWAs (multiple employer welfare arrangements), association plans and church plans-in addition to government entities permitted to self fund, which includes the NJ State Health Benefit Program, HIFs, counties, municipalities and agencies.
Only the Beginning?
Patient protection is always the goal. But it did not have to be this way. Or so complicated.
Inclusion of the Medicare Allowable Charge upon all billing (a current federal proposal) would have benchmarked the relative value the act clumsily mishandles. The existing statute regarding excessive fees could have been modified to declare charges in excess of "x" times the Medicare Allowable Charge to be de facto excessive and barred. Alternatively, a requirement could have been made that all contracted services to hospitals and all employee physicians of a hospital mirror its participation status.
Instead, the act is hastily written, contradicting itself at times, ignoring existing state and federal claims handling and appeal rights. Conflict of laws and federal pre-emption challenges will plague implementation. The data lift of carriers and providers is substantial. The authority in arbitration to exceed stated out-of-network plan limits is unknown, but doubtful. The significance of "plans" not being synonymous with "carriers" is completely missed. Whether estimation of costs will operate as a medical version of a mechanic's pre-estimate is unsettled. Claims negotiation services are constrained due to the new processing deadlines. Because such cost saving mechanisms are curtailed, self-funded plans may be disproportionately affected, particularly those sponsored by municipalities, counties and unions.
It did not have to be this way. Or so complicated.State to Enforce "Shared Responsibility Tax"
Monday, June 11, 2018 Craig Chapin
 NJ Governor Phil Murphy wants money, if residents don't maintain individual health insurance. Effective January 1, 2019, the governor signed a new law reestablishing the recently repealed "shared responsibly tax". It forces individuals to pay 2.5 percent of a household's income or a per-person charge - whichever is higher. A "hardship exception" for individuals who cannot afford coverage would be decided by one person i.e. the state treasurer Elizabeth Mucio.
NJ Governor Phil Murphy wants money, if residents don't maintain individual health insurance. Effective January 1, 2019, the governor signed a new law reestablishing the recently repealed "shared responsibly tax". It forces individuals to pay 2.5 percent of a household's income or a per-person charge - whichever is higher. A "hardship exception" for individuals who cannot afford coverage would be decided by one person i.e. the state treasurer Elizabeth Mucio.
At the same time, NJ is one of the worst states for offering individual alternatives to fill the gaps in the out-of-pocket cost for health insurance. NJ also does not allow individuals to secure short term major medical in-between open enrollment periods.
The maximum out-of-pocket cost for health insurance will be raised, based on the inflation-adjusted out-of-pocket limits from $7,350 per individual and $14,700 per family to $7,900 per individual and $15,800 per family in 2019. Meanwhile, according to the Kaiser Family Foundation (KFF), more than a quarter of U.S. adults struggle to pay their medical bills. This includes folks who have insurance, whether independently or through an employer. In fact, medical debt is the No. 1 source of personal bankruptcy filings in the U.S.. In 2014, an estimated 40% of Americans racked up debt resulting from a medical issue. The amount of money owed on average is $13,279 based on a 2007 study. Moreover, according to a recent GoBankingRates survey, 69% of Americans have less than $1,000 in savings, while 34% have no money in the bank whatsoever.
The options are slim to none if you do not have coverage or you lapse your insurance for non-payment of premium. We have been giving individuals with no coverage a way to offset medical expenses based on four services. Access to doc 24/7, broach certified doctors who can prescribe medication, accident plans that pay up to $15,000 per individual based on billed charges, Preferred Provider access to any type of medical expenses allowing you to pay wholesale verses retail rates, life with living benefits of critical, chronic, and Long Term Care protection. Term and Permanent life insurance can advance pay the death benefits for major medical conditions that shorten one's life span.
Everyone should beware of the law when you can enroll and the options available to them. Most people are not aware that each family member can enroll in a different health plan, based on their needs. Some still do not realize that children can be covered for low or no cost through the state children health program. I also find that most people do not know the rules that allow them to qualify for substantial subsidies on individual insurance. They are also unfamiliar with the ways they could take advantage of tax savings for no covered out-of-pocket medical, vision, and dental expenses.
There are numerous other rules and requirements that individual and employers should know as well. Everyone needs to have a trained advisor. Everyone needs to know that a Navigator or the Marketplace representatives are not licensed, cannot discuss insurance plans, and typically just go by what their computer tells them. There is a tremendous amount that you need to be advised on when protecting your family and more changes are coming.
Recent executive orders from the White House will allow for association plans to be marketed. These plans will not offer all the essential services required by the Affordable Care Act. Therefore, you will have to read the contracts to find out what is not included. Buyers beware!
 NJ Governor Phil Murphy wants money, if residents don't maintain individual health insurance. Effective January 1, 2019, the governor signed a new law reestablishing the recently repealed "shared responsibly tax". It forces individuals to pay 2.5 percent of a household's income or a per-person charge - whichever is higher. A "hardship exception" for individuals who cannot afford coverage would be decided by one person i.e. the state treasurer Elizabeth Mucio.
NJ Governor Phil Murphy wants money, if residents don't maintain individual health insurance. Effective January 1, 2019, the governor signed a new law reestablishing the recently repealed "shared responsibly tax". It forces individuals to pay 2.5 percent of a household's income or a per-person charge - whichever is higher. A "hardship exception" for individuals who cannot afford coverage would be decided by one person i.e. the state treasurer Elizabeth Mucio. At the same time, NJ is one of the worst states for offering individual alternatives to fill the gaps in the out-of-pocket cost for health insurance. NJ also does not allow individuals to secure short term major medical in-between open enrollment periods.
The maximum out-of-pocket cost for health insurance will be raised, based on the inflation-adjusted out-of-pocket limits from $7,350 per individual and $14,700 per family to $7,900 per individual and $15,800 per family in 2019. Meanwhile, according to the Kaiser Family Foundation (KFF), more than a quarter of U.S. adults struggle to pay their medical bills. This includes folks who have insurance, whether independently or through an employer. In fact, medical debt is the No. 1 source of personal bankruptcy filings in the U.S.. In 2014, an estimated 40% of Americans racked up debt resulting from a medical issue. The amount of money owed on average is $13,279 based on a 2007 study. Moreover, according to a recent GoBankingRates survey, 69% of Americans have less than $1,000 in savings, while 34% have no money in the bank whatsoever.
The options are slim to none if you do not have coverage or you lapse your insurance for non-payment of premium. We have been giving individuals with no coverage a way to offset medical expenses based on four services. Access to doc 24/7, broach certified doctors who can prescribe medication, accident plans that pay up to $15,000 per individual based on billed charges, Preferred Provider access to any type of medical expenses allowing you to pay wholesale verses retail rates, life with living benefits of critical, chronic, and Long Term Care protection. Term and Permanent life insurance can advance pay the death benefits for major medical conditions that shorten one's life span.
Everyone should beware of the law when you can enroll and the options available to them. Most people are not aware that each family member can enroll in a different health plan, based on their needs. Some still do not realize that children can be covered for low or no cost through the state children health program. I also find that most people do not know the rules that allow them to qualify for substantial subsidies on individual insurance. They are also unfamiliar with the ways they could take advantage of tax savings for no covered out-of-pocket medical, vision, and dental expenses.
There are numerous other rules and requirements that individual and employers should know as well. Everyone needs to have a trained advisor. Everyone needs to know that a Navigator or the Marketplace representatives are not licensed, cannot discuss insurance plans, and typically just go by what their computer tells them. There is a tremendous amount that you need to be advised on when protecting your family and more changes are coming.
Recent executive orders from the White House will allow for association plans to be marketed. These plans will not offer all the essential services required by the Affordable Care Act. Therefore, you will have to read the contracts to find out what is not included. Buyers beware!
Paid Sick Leave Starts 10/29/2018
Thursday, June 07, 2018 Craig Chapin
 The new law applies to any business entity in NJ that hires employees regardless of its size. The law is broad-based in coverage and will surely hurt employers with high turnover positions. NJ will be following nine other states that are the only ones to implement this benefit. This adds to the already high burden on employers in NJ. The Paid Sick Leave law excludes employers in the construction industry employed by union, per diem healthcare employees, and public employers who must give paid sick leave to their employees. Furthermore, this law supersedes all existing and any future municipal ordinances in the state that deal with paid sick leave. Tax payers will pick up the costs for the municipalities and employers will have to pass on the cost to their customers.
The new law applies to any business entity in NJ that hires employees regardless of its size. The law is broad-based in coverage and will surely hurt employers with high turnover positions. NJ will be following nine other states that are the only ones to implement this benefit. This adds to the already high burden on employers in NJ. The Paid Sick Leave law excludes employers in the construction industry employed by union, per diem healthcare employees, and public employers who must give paid sick leave to their employees. Furthermore, this law supersedes all existing and any future municipal ordinances in the state that deal with paid sick leave. Tax payers will pick up the costs for the municipalities and employers will have to pass on the cost to their customers.
The law allows employees to accrue sick leave time with a cap of 40 hours per benefit year at a rate of 1 hour for every 30 hours worked. Employer can frontload said hours at the beginning of the company's designated benefits year. Although, I do not think there will be many takers. Additionally, employers who have existing PTO, personal days, vacation days, and sick day policies may utilize them to meet the requirements set by the state paid sick leave law. All existing policies have to meet the state law requirements.
Employer can subtract part-time and seasonal workers that work less than 120 days for the company. However, once this waiting period is met, employees can use paid sick time for these reasons:
Questions remain. For instance, does a NJ employer have to offer the same benefits to out-of-state employees working for the NJ employer? Can they instead avoid the policy with an independent contractor designation? Even temporary help service firms are affected as the paid sick leave will accrue by the total time worked on assignment. Employers are instructed to seek assistance from HR compliance experts to help prepare for the law and ensure compliance when it goes into effect.
 The new law applies to any business entity in NJ that hires employees regardless of its size. The law is broad-based in coverage and will surely hurt employers with high turnover positions. NJ will be following nine other states that are the only ones to implement this benefit. This adds to the already high burden on employers in NJ. The Paid Sick Leave law excludes employers in the construction industry employed by union, per diem healthcare employees, and public employers who must give paid sick leave to their employees. Furthermore, this law supersedes all existing and any future municipal ordinances in the state that deal with paid sick leave. Tax payers will pick up the costs for the municipalities and employers will have to pass on the cost to their customers.
The new law applies to any business entity in NJ that hires employees regardless of its size. The law is broad-based in coverage and will surely hurt employers with high turnover positions. NJ will be following nine other states that are the only ones to implement this benefit. This adds to the already high burden on employers in NJ. The Paid Sick Leave law excludes employers in the construction industry employed by union, per diem healthcare employees, and public employers who must give paid sick leave to their employees. Furthermore, this law supersedes all existing and any future municipal ordinances in the state that deal with paid sick leave. Tax payers will pick up the costs for the municipalities and employers will have to pass on the cost to their customers.The law allows employees to accrue sick leave time with a cap of 40 hours per benefit year at a rate of 1 hour for every 30 hours worked. Employer can frontload said hours at the beginning of the company's designated benefits year. Although, I do not think there will be many takers. Additionally, employers who have existing PTO, personal days, vacation days, and sick day policies may utilize them to meet the requirements set by the state paid sick leave law. All existing policies have to meet the state law requirements.
Employer can subtract part-time and seasonal workers that work less than 120 days for the company. However, once this waiting period is met, employees can use paid sick time for these reasons:
- The diagnosis, treatment, and recovery from a mental or physical illness (preventive medical care included)
- Caring for a covered family member during the diagnosis, treatment, and recovery from mental or physical illness (preventative medical care included)
- Recovering from domestic or sexual violence (either an employee or an employee's family member)
- The closing of an employee's workplace due to a public health emergency
- The closing of a school of an employee's child due to a public health emergency
- Attending school conferences or meetings to discuss a child's health condition or disability
Questions remain. For instance, does a NJ employer have to offer the same benefits to out-of-state employees working for the NJ employer? Can they instead avoid the policy with an independent contractor designation? Even temporary help service firms are affected as the paid sick leave will accrue by the total time worked on assignment. Employers are instructed to seek assistance from HR compliance experts to help prepare for the law and ensure compliance when it goes into effect.
Health Care: Brace for shorter enrollment season and higher rates
Wednesday, September 06, 2017
 Rates have been filed across the country and the outlook is not great. Not only will individuals have to sign up for coverage within 45 days, but the choice will also be limited. Across the nation, 42.41% of counties will only have one insurance carrier to pick a plan with and 1.27% of counties are projected to have no carriers at all. Premium rates for larger networks of providers or offering out-of-state or out-of-network coverage will increase upwards of 59%. Meanwhile, the maximum out-of-pocket cost for individuals and groups will be raised to $7,350 for self-only coverage and $14,700 for family coverage.
Still, upwards of three-quarters of individuals will be insulated from rate hikes by staying with the high out-of-pocket benchmark plans using the subsidies offered through the Affordable Care Act. Individuals earning less than 250% of the Federal Poverty Level will also be shielded from higher out of pocket costs unless of course, President Trumps stops the cost sharing subsidies.
As of this date, it looks like individuals earning over 400% of the Federal Poverty Level will pay an average increase of 22% with Horizon of New Jersey on their popular Omnia Silver plan. AmeriHealth is asking for as much as a 59% increase on some plans. Eastern PA residents seem to be spared with Keystone Health Plan East looking for a 4.6% increase on individuals but 10.18% on small group plans. In New York, the average increase is 14.6% for individuals and 9.3% for small groups plans. Looking at these price increases, it is strange that Eastern PA, with only one insurance carrier, is offering coverage with the lowest rate increase while NJ, with 3 carriers, and NY, with 15, cannot say the same. Still, these rate increases on top of last year's increase will make insurance unfordable to many paying the full cost for coverage.
1 Stop Benefits Inc. will continue to stay on top of all the changes in the insurance world, and seek out ways to find high quality, low-cost care for everyone. We strongly suggest you contact us right away and as about our enhanced supplements to fill the gaps in any health plan. Some of these low-cost cash benefits will not be available to new clients as of the new open enrollment. NJ residents should view this Flyer because you only have up to November 15 to purchase.
Rates have been filed across the country and the outlook is not great. Not only will individuals have to sign up for coverage within 45 days, but the choice will also be limited. Across the nation, 42.41% of counties will only have one insurance carrier to pick a plan with and 1.27% of counties are projected to have no carriers at all. Premium rates for larger networks of providers or offering out-of-state or out-of-network coverage will increase upwards of 59%. Meanwhile, the maximum out-of-pocket cost for individuals and groups will be raised to $7,350 for self-only coverage and $14,700 for family coverage.
Still, upwards of three-quarters of individuals will be insulated from rate hikes by staying with the high out-of-pocket benchmark plans using the subsidies offered through the Affordable Care Act. Individuals earning less than 250% of the Federal Poverty Level will also be shielded from higher out of pocket costs unless of course, President Trumps stops the cost sharing subsidies.
As of this date, it looks like individuals earning over 400% of the Federal Poverty Level will pay an average increase of 22% with Horizon of New Jersey on their popular Omnia Silver plan. AmeriHealth is asking for as much as a 59% increase on some plans. Eastern PA residents seem to be spared with Keystone Health Plan East looking for a 4.6% increase on individuals but 10.18% on small group plans. In New York, the average increase is 14.6% for individuals and 9.3% for small groups plans. Looking at these price increases, it is strange that Eastern PA, with only one insurance carrier, is offering coverage with the lowest rate increase while NJ, with 3 carriers, and NY, with 15, cannot say the same. Still, these rate increases on top of last year's increase will make insurance unfordable to many paying the full cost for coverage.
1 Stop Benefits Inc. will continue to stay on top of all the changes in the insurance world, and seek out ways to find high quality, low-cost care for everyone. We strongly suggest you contact us right away and as about our enhanced supplements to fill the gaps in any health plan. Some of these low-cost cash benefits will not be available to new clients as of the new open enrollment. NJ residents should view this Flyer because you only have up to November 15 to purchase.
 Rates have been filed across the country and the outlook is not great. Not only will individuals have to sign up for coverage within 45 days, but the choice will also be limited. Across the nation, 42.41% of counties will only have one insurance carrier to pick a plan with and 1.27% of counties are projected to have no carriers at all. Premium rates for larger networks of providers or offering out-of-state or out-of-network coverage will increase upwards of 59%. Meanwhile, the maximum out-of-pocket cost for individuals and groups will be raised to $7,350 for self-only coverage and $14,700 for family coverage.
Still, upwards of three-quarters of individuals will be insulated from rate hikes by staying with the high out-of-pocket benchmark plans using the subsidies offered through the Affordable Care Act. Individuals earning less than 250% of the Federal Poverty Level will also be shielded from higher out of pocket costs unless of course, President Trumps stops the cost sharing subsidies.
As of this date, it looks like individuals earning over 400% of the Federal Poverty Level will pay an average increase of 22% with Horizon of New Jersey on their popular Omnia Silver plan. AmeriHealth is asking for as much as a 59% increase on some plans. Eastern PA residents seem to be spared with Keystone Health Plan East looking for a 4.6% increase on individuals but 10.18% on small group plans. In New York, the average increase is 14.6% for individuals and 9.3% for small groups plans. Looking at these price increases, it is strange that Eastern PA, with only one insurance carrier, is offering coverage with the lowest rate increase while NJ, with 3 carriers, and NY, with 15, cannot say the same. Still, these rate increases on top of last year's increase will make insurance unfordable to many paying the full cost for coverage.
1 Stop Benefits Inc. will continue to stay on top of all the changes in the insurance world, and seek out ways to find high quality, low-cost care for everyone. We strongly suggest you contact us right away and as about our enhanced supplements to fill the gaps in any health plan. Some of these low-cost cash benefits will not be available to new clients as of the new open enrollment. NJ residents should view this Flyer because you only have up to November 15 to purchase.
Rates have been filed across the country and the outlook is not great. Not only will individuals have to sign up for coverage within 45 days, but the choice will also be limited. Across the nation, 42.41% of counties will only have one insurance carrier to pick a plan with and 1.27% of counties are projected to have no carriers at all. Premium rates for larger networks of providers or offering out-of-state or out-of-network coverage will increase upwards of 59%. Meanwhile, the maximum out-of-pocket cost for individuals and groups will be raised to $7,350 for self-only coverage and $14,700 for family coverage.
Still, upwards of three-quarters of individuals will be insulated from rate hikes by staying with the high out-of-pocket benchmark plans using the subsidies offered through the Affordable Care Act. Individuals earning less than 250% of the Federal Poverty Level will also be shielded from higher out of pocket costs unless of course, President Trumps stops the cost sharing subsidies.
As of this date, it looks like individuals earning over 400% of the Federal Poverty Level will pay an average increase of 22% with Horizon of New Jersey on their popular Omnia Silver plan. AmeriHealth is asking for as much as a 59% increase on some plans. Eastern PA residents seem to be spared with Keystone Health Plan East looking for a 4.6% increase on individuals but 10.18% on small group plans. In New York, the average increase is 14.6% for individuals and 9.3% for small groups plans. Looking at these price increases, it is strange that Eastern PA, with only one insurance carrier, is offering coverage with the lowest rate increase while NJ, with 3 carriers, and NY, with 15, cannot say the same. Still, these rate increases on top of last year's increase will make insurance unfordable to many paying the full cost for coverage.
1 Stop Benefits Inc. will continue to stay on top of all the changes in the insurance world, and seek out ways to find high quality, low-cost care for everyone. We strongly suggest you contact us right away and as about our enhanced supplements to fill the gaps in any health plan. Some of these low-cost cash benefits will not be available to new clients as of the new open enrollment. NJ residents should view this Flyer because you only have up to November 15 to purchase.Everyone loves a sale... Save on your medical/dental coverage!
Wednesday, September 06, 2017
 We can see this in the news all of the time. For example, the recent merger of Amazon with Whole Foods has sent many, including the media, into lively discussions about price cuts and possible Amazon Prime benefits.
Many times, we see the purchase of an item or service being justified by its sale pricing. I often ask my children, "a sale on what?" After all, sales often follow after price hikes on items, making a sale seem to be a bigger discount than it ever really was. Marketers use the word "sale" to evoke quick decision thinking, and while this tactic has been used forever, we still fall into the notion that we are getting a bargain.
Using the word "Sale" in the medical or dental industry does not have the same impact to drive a reaction. Most people would not have a surgery because the treatment was discounted. The majority of us also would not sign up for another dental cleaning just because there was a discounted rate.
So, the fact that anyone can get a discount when obtaining medical or dental care does not motivate an immediate reaction. You may react quickly to a medical device or vitamin on sale, but you are more likely to schedule a yearly physical based on your insurance plan offerings. While everyone would prefer better health or cleaner teeth, many label the treatment and maintenance required as too costly.
Part of this problem in the medical/dental world is lack of awareness of the cost of care. The average person has no idea if the price they are paying for healthcare is reasonable. Moreover, people develop relationships with their dentist or doctor, making shopping for affordable care more complicated.
With the right insurance coverage, every family can find a true "sale" on medical/dental care. Discounts in the world of health care do exist (and never at the expense of quality!). Being better informed about the costs of your providers and the benefits of your insurance plans can help you always get the most for your money. Give a 1 Stop Benefits representative a call and ask about the WellCard Saving program and our pricing links to find out what is a reasonable cost for any type treatment or prescription in your area. Click to call.
We can see this in the news all of the time. For example, the recent merger of Amazon with Whole Foods has sent many, including the media, into lively discussions about price cuts and possible Amazon Prime benefits.
Many times, we see the purchase of an item or service being justified by its sale pricing. I often ask my children, "a sale on what?" After all, sales often follow after price hikes on items, making a sale seem to be a bigger discount than it ever really was. Marketers use the word "sale" to evoke quick decision thinking, and while this tactic has been used forever, we still fall into the notion that we are getting a bargain.
Using the word "Sale" in the medical or dental industry does not have the same impact to drive a reaction. Most people would not have a surgery because the treatment was discounted. The majority of us also would not sign up for another dental cleaning just because there was a discounted rate.
So, the fact that anyone can get a discount when obtaining medical or dental care does not motivate an immediate reaction. You may react quickly to a medical device or vitamin on sale, but you are more likely to schedule a yearly physical based on your insurance plan offerings. While everyone would prefer better health or cleaner teeth, many label the treatment and maintenance required as too costly.
Part of this problem in the medical/dental world is lack of awareness of the cost of care. The average person has no idea if the price they are paying for healthcare is reasonable. Moreover, people develop relationships with their dentist or doctor, making shopping for affordable care more complicated.
With the right insurance coverage, every family can find a true "sale" on medical/dental care. Discounts in the world of health care do exist (and never at the expense of quality!). Being better informed about the costs of your providers and the benefits of your insurance plans can help you always get the most for your money. Give a 1 Stop Benefits representative a call and ask about the WellCard Saving program and our pricing links to find out what is a reasonable cost for any type treatment or prescription in your area. Click to call.
 We can see this in the news all of the time. For example, the recent merger of Amazon with Whole Foods has sent many, including the media, into lively discussions about price cuts and possible Amazon Prime benefits.
Many times, we see the purchase of an item or service being justified by its sale pricing. I often ask my children, "a sale on what?" After all, sales often follow after price hikes on items, making a sale seem to be a bigger discount than it ever really was. Marketers use the word "sale" to evoke quick decision thinking, and while this tactic has been used forever, we still fall into the notion that we are getting a bargain.
Using the word "Sale" in the medical or dental industry does not have the same impact to drive a reaction. Most people would not have a surgery because the treatment was discounted. The majority of us also would not sign up for another dental cleaning just because there was a discounted rate.
So, the fact that anyone can get a discount when obtaining medical or dental care does not motivate an immediate reaction. You may react quickly to a medical device or vitamin on sale, but you are more likely to schedule a yearly physical based on your insurance plan offerings. While everyone would prefer better health or cleaner teeth, many label the treatment and maintenance required as too costly.
Part of this problem in the medical/dental world is lack of awareness of the cost of care. The average person has no idea if the price they are paying for healthcare is reasonable. Moreover, people develop relationships with their dentist or doctor, making shopping for affordable care more complicated.
With the right insurance coverage, every family can find a true "sale" on medical/dental care. Discounts in the world of health care do exist (and never at the expense of quality!). Being better informed about the costs of your providers and the benefits of your insurance plans can help you always get the most for your money. Give a 1 Stop Benefits representative a call and ask about the WellCard Saving program and our pricing links to find out what is a reasonable cost for any type treatment or prescription in your area. Click to call.
We can see this in the news all of the time. For example, the recent merger of Amazon with Whole Foods has sent many, including the media, into lively discussions about price cuts and possible Amazon Prime benefits.
Many times, we see the purchase of an item or service being justified by its sale pricing. I often ask my children, "a sale on what?" After all, sales often follow after price hikes on items, making a sale seem to be a bigger discount than it ever really was. Marketers use the word "sale" to evoke quick decision thinking, and while this tactic has been used forever, we still fall into the notion that we are getting a bargain.
Using the word "Sale" in the medical or dental industry does not have the same impact to drive a reaction. Most people would not have a surgery because the treatment was discounted. The majority of us also would not sign up for another dental cleaning just because there was a discounted rate.
So, the fact that anyone can get a discount when obtaining medical or dental care does not motivate an immediate reaction. You may react quickly to a medical device or vitamin on sale, but you are more likely to schedule a yearly physical based on your insurance plan offerings. While everyone would prefer better health or cleaner teeth, many label the treatment and maintenance required as too costly.
Part of this problem in the medical/dental world is lack of awareness of the cost of care. The average person has no idea if the price they are paying for healthcare is reasonable. Moreover, people develop relationships with their dentist or doctor, making shopping for affordable care more complicated.
With the right insurance coverage, every family can find a true "sale" on medical/dental care. Discounts in the world of health care do exist (and never at the expense of quality!). Being better informed about the costs of your providers and the benefits of your insurance plans can help you always get the most for your money. Give a 1 Stop Benefits representative a call and ask about the WellCard Saving program and our pricing links to find out what is a reasonable cost for any type treatment or prescription in your area. Click to call.Calculating Life Expectancy: Planning For Your Future
Wednesday, September 06, 2017
 The average American male lives to age the age of 84 while the average female lives to 86 years old. Of course, these estimates do not take into consideration family history or personal life habits. We recommend checking out an online life expectancy calculator to take into consideration your unique circumstances. Either way, Americans in general lead long lives - and we certainly do not expect ourselves to work all of those years. This is why planning for retirement as early as possible is important.
While we may be living longer, more and more individuals are being diagnosed with chronic health conditions. Over 40% of individuals will have at least one chronic condition diagnosed before the age of 65, and 70% of individuals will need long-term care sometime in their lifetime. With the high likelihood of a critical, chronic or long-term health care expense, there is great need to plan ahead to offset those exuberant costs. Unfortunately, government resources cannot be relied upon in the future - with programs like Medicare, Medicaid, and Social Security facing huge funding issues.
You may already be aware that insurance plans exist to cover the cost of long term and critical illness care. It may be difficult to think about purchasing such care. Many believe it to be expensive or unnecessary. However, one just needs to look around to family, friends, and neighbors to see individuals suffering from the financial impact of unexpected medical treatment and assisted care.
The viatical and senior settlement business rose out of the need for terminally individuals to gain additional money to cover their excessive medical costs. Terminally ill individuals sell their life insurance coverage in order to support themselves. However, a new form of life insurance has recently emerged and offers living cash benefits as a part of the policy.
Living benefits built into a low-cost term and permanent life insurance gives younger adults a huge reason to purchase coverage now, especially because there is no telling what the future holds. This coverage is not a replacement for the purchase of disability or long-term care insurance, as those plans offer much more robust cash benefits as a result of short term illnesses or non-life altering conditions, especially during one's earning years. However, purchasing a life insurance policy with living cash benefits may help reduce some of the burdens we all may face as we grow older. To learn more about life insurance with living cash benefits- talk to us at 1 Stop Benefits Inc.
The average American male lives to age the age of 84 while the average female lives to 86 years old. Of course, these estimates do not take into consideration family history or personal life habits. We recommend checking out an online life expectancy calculator to take into consideration your unique circumstances. Either way, Americans in general lead long lives - and we certainly do not expect ourselves to work all of those years. This is why planning for retirement as early as possible is important.
While we may be living longer, more and more individuals are being diagnosed with chronic health conditions. Over 40% of individuals will have at least one chronic condition diagnosed before the age of 65, and 70% of individuals will need long-term care sometime in their lifetime. With the high likelihood of a critical, chronic or long-term health care expense, there is great need to plan ahead to offset those exuberant costs. Unfortunately, government resources cannot be relied upon in the future - with programs like Medicare, Medicaid, and Social Security facing huge funding issues.
You may already be aware that insurance plans exist to cover the cost of long term and critical illness care. It may be difficult to think about purchasing such care. Many believe it to be expensive or unnecessary. However, one just needs to look around to family, friends, and neighbors to see individuals suffering from the financial impact of unexpected medical treatment and assisted care.
The viatical and senior settlement business rose out of the need for terminally individuals to gain additional money to cover their excessive medical costs. Terminally ill individuals sell their life insurance coverage in order to support themselves. However, a new form of life insurance has recently emerged and offers living cash benefits as a part of the policy.
Living benefits built into a low-cost term and permanent life insurance gives younger adults a huge reason to purchase coverage now, especially because there is no telling what the future holds. This coverage is not a replacement for the purchase of disability or long-term care insurance, as those plans offer much more robust cash benefits as a result of short term illnesses or non-life altering conditions, especially during one's earning years. However, purchasing a life insurance policy with living cash benefits may help reduce some of the burdens we all may face as we grow older. To learn more about life insurance with living cash benefits- talk to us at 1 Stop Benefits Inc.
 The average American male lives to age the age of 84 while the average female lives to 86 years old. Of course, these estimates do not take into consideration family history or personal life habits. We recommend checking out an online life expectancy calculator to take into consideration your unique circumstances. Either way, Americans in general lead long lives - and we certainly do not expect ourselves to work all of those years. This is why planning for retirement as early as possible is important.
While we may be living longer, more and more individuals are being diagnosed with chronic health conditions. Over 40% of individuals will have at least one chronic condition diagnosed before the age of 65, and 70% of individuals will need long-term care sometime in their lifetime. With the high likelihood of a critical, chronic or long-term health care expense, there is great need to plan ahead to offset those exuberant costs. Unfortunately, government resources cannot be relied upon in the future - with programs like Medicare, Medicaid, and Social Security facing huge funding issues.
You may already be aware that insurance plans exist to cover the cost of long term and critical illness care. It may be difficult to think about purchasing such care. Many believe it to be expensive or unnecessary. However, one just needs to look around to family, friends, and neighbors to see individuals suffering from the financial impact of unexpected medical treatment and assisted care.
The viatical and senior settlement business rose out of the need for terminally individuals to gain additional money to cover their excessive medical costs. Terminally ill individuals sell their life insurance coverage in order to support themselves. However, a new form of life insurance has recently emerged and offers living cash benefits as a part of the policy.
Living benefits built into a low-cost term and permanent life insurance gives younger adults a huge reason to purchase coverage now, especially because there is no telling what the future holds. This coverage is not a replacement for the purchase of disability or long-term care insurance, as those plans offer much more robust cash benefits as a result of short term illnesses or non-life altering conditions, especially during one's earning years. However, purchasing a life insurance policy with living cash benefits may help reduce some of the burdens we all may face as we grow older. To learn more about life insurance with living cash benefits- talk to us at 1 Stop Benefits Inc.
The average American male lives to age the age of 84 while the average female lives to 86 years old. Of course, these estimates do not take into consideration family history or personal life habits. We recommend checking out an online life expectancy calculator to take into consideration your unique circumstances. Either way, Americans in general lead long lives - and we certainly do not expect ourselves to work all of those years. This is why planning for retirement as early as possible is important.
While we may be living longer, more and more individuals are being diagnosed with chronic health conditions. Over 40% of individuals will have at least one chronic condition diagnosed before the age of 65, and 70% of individuals will need long-term care sometime in their lifetime. With the high likelihood of a critical, chronic or long-term health care expense, there is great need to plan ahead to offset those exuberant costs. Unfortunately, government resources cannot be relied upon in the future - with programs like Medicare, Medicaid, and Social Security facing huge funding issues.
You may already be aware that insurance plans exist to cover the cost of long term and critical illness care. It may be difficult to think about purchasing such care. Many believe it to be expensive or unnecessary. However, one just needs to look around to family, friends, and neighbors to see individuals suffering from the financial impact of unexpected medical treatment and assisted care.
The viatical and senior settlement business rose out of the need for terminally individuals to gain additional money to cover their excessive medical costs. Terminally ill individuals sell their life insurance coverage in order to support themselves. However, a new form of life insurance has recently emerged and offers living cash benefits as a part of the policy.
Living benefits built into a low-cost term and permanent life insurance gives younger adults a huge reason to purchase coverage now, especially because there is no telling what the future holds. This coverage is not a replacement for the purchase of disability or long-term care insurance, as those plans offer much more robust cash benefits as a result of short term illnesses or non-life altering conditions, especially during one's earning years. However, purchasing a life insurance policy with living cash benefits may help reduce some of the burdens we all may face as we grow older. To learn more about life insurance with living cash benefits- talk to us at 1 Stop Benefits Inc.
- Check out the Social Security Estimator.
- Watch our Video and Learn More.
